Introduction
Everyone of us has experienced wobbly teeth during our childhood, especially when our milk teeth have started to fall out. Such event is considered to be physiologic as the milk teeth are giving ways for our permanent teeth to grow. The milk teeth or primary dentition will undergo gradual root resorption which is stimulated by the developing permanent tooth underneath. Eventually, the milk teeth will exfoliate and will be replaced by permanent teeth or secondary dentition.
Contrarily, having loose or mobile teeth in adult can be quite a daunting experience. Such event is not considered to be physiologic. In fact, it is mostly an indicator of disease progression. Permanent dentition can become loose for a number of reasons, including trauma, grinding, biting on hard things, or periodontal/gum disease.
|
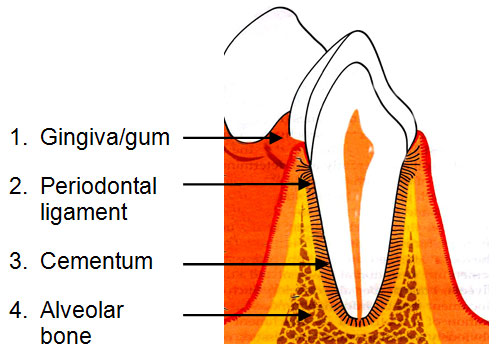
Periodontium consists of four component :
Periodontium is also known as attachment apparatus or supporting tissues. Loose teeth or tooth mobility can be defined as the movement of tooth/teeth in the socket, usually resulting from inadequate bone support. |
There are two types of tooth mobility
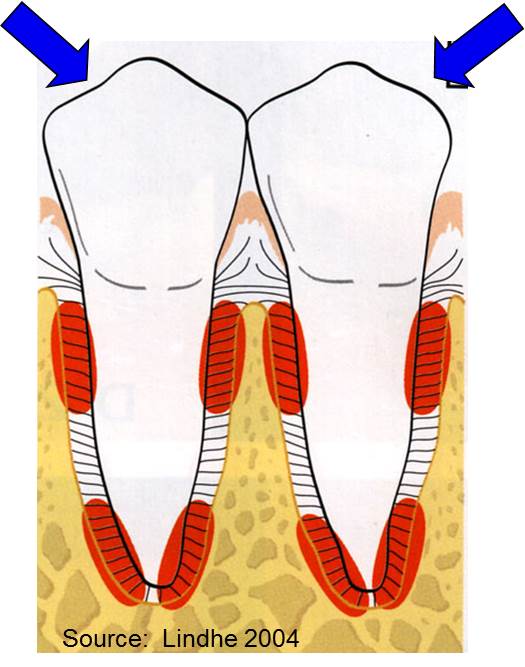
- Physiologic – It is considered as natural tooth mobility. The tooth is attached to the jaw bones or sockets by a special ligament. This ligament will allow slight mobility to accommodate forces on the teeth during jaw function, like chewing or biting.
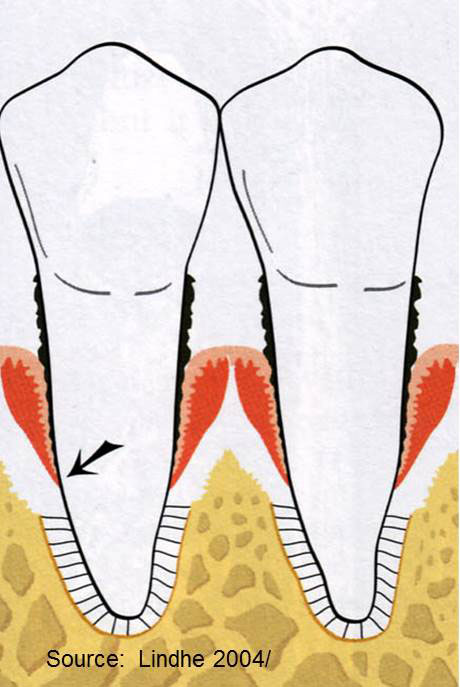
- Pathologic or abnormal tooth mobility occurred when the attachment of the periodontal ligament is destroyed due to factors like inflammation and infection of bacteria. The degree of mobility is depending on the amount of bone and periodontal ligament support remained.
Causes of Tooth Mobility
Trauma from Injury
If a tooth is traumatized due to fall injury especially in children or motor vehicle accident, the tooth may become mobile. Depending on the severity of the injury, some cases may not need treatment as the tooth ligament may tighten up again by itself. Nerve injury is common complication following trauma to the tooth. Having symptoms of hypersensitivity, extreme pain and swelling with pus draining out, might warrant nerve treatment of the tooth. Therefore, it is advisable to seek dental treatment in order to rule out any possible complications.
Occlusal or biting trauma
Occurs when there is an injury to the ligament, resulting from excessive biting forces applied to a tooth or teeth. For examples, high filling and faulty restorations will cause excessive force on the opposing teeth. Occlusal trauma can also occur in patient with less tooth bone support, such as periodontal disease. In this situation, whether the biting force is normal or excessive, the tooth is more prone to be affected. If periodontal disease is present together with excessive force, more damage may occur.
Bruxism or teeth grinding habit can lead to tooth mobility due to excessive forces between upper and lower teeth. Tooth mobility will not occur if there is attrition on the tooth surface. Bruxism will worsen the tissue attachment loss if periodontal disease is already present. Tooth mobility will not progress if grinding habit is under control and under proper management and guidance.
Tumour or growth
In rare cases, unexplained tooth mobility may indicate tumour of the jaw, in particular tumour that is destructing the periodontal supporting tissues. Further investigation is needed to exclude this condition.
Signs and Symptoms
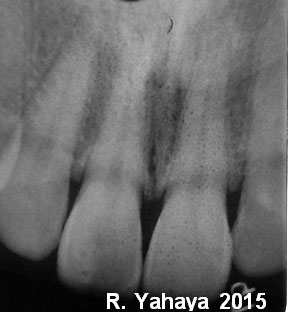
Tooth mobility is not a disease per se; it is actually a sign and symptom of other condition or diseases. The specialist or Dentist should investigate for the cause. The severity of tooth mobility is based on the total amount of bone loss (see two x-ray pictures below which indicates normal bone height and more than half of the root length of bone loss on upper incisor teeth due to periodontal disease).
Tooth mobility are classified by grading system; it can be either Grade 1, when the tooth can be moved in horizontal plane less than 1mm; or Grade 2, where the tooth can be moved 1 mm or more; or the worst, Grade 3, where the tooth can be moved 1 mm or more with vertical direction.
Other than tooth mobility, patient with periodontal disease may also exhibit:
- Gum recession;
- Swollen gum, sometimes with pus formation (suppuration) and discharge;
- Gum inflammation (Redness of gum);
- Drifting teeth;
- Tooth pain;
- Bleeding gums;
- Tooth Sensitivity to hot or cold drink/food
If you notice that you have any of the above mentioned signs or symptoms, you may want to visit your dentist as soon as possible in order to avoid further progression of tooth mobility or advanced stage of periodontitis.
In cases of occlusal trauma, signs and symptoms that the patient and the dentist can look for include progressive mobility, wear facets, tooth migration on one tooth or more, thermal sensitivity and fractured tooth.
Complications
Patient with tooth mobility will usually have discomfort and difficulty upon chewing or biting, and in worst-case scenario, if left untreated; it will lead to tooth loss as support from the bone is inadequate.
Treatment
In the absence of infection or periodontal disease, if the cause of tooth mobility is removed the tooth will re-gain strength. If you have been diagnosed to have periodontal disease, your dentist will usually refer you to the nearest Periodontist (A Gum Specialist). In Malaysia, every state has at least one Periodontist to cater the periodontal treatment need of the patients.
Oral Hygiene care guidance and removal of harmful bacteria via scaling and root debridement (deep cleaning on the root surface to remove plaque and calculus) are examples of treatment that will be carried out. You need to adhere to the treatment protocol which includes non-surgical, surgical and maintenance phase of treatment.
Occlusal trauma cases are usually treated by occlusal adjustment therapy. Occlusal adjustment can be achieved through selective grinding of the high bite spot whereas in severe case, orthodontic treatment (braces treatment) by adjusting misaligned position of the teeth is necessary.
If the tooth is mobile, splinting can be done to immobilize teeth in order to allow healing process after deep cleaning and to increase comfort during chewing activity. Splinting is a procedure that joins two or more teeth using either a special wire or an appliance. It is usually indicated in grade 2 and 3 mobility where progression of severity is observed in certain period of time. Teeth are thus immobilized and occlusal forces are better distributed. However, it depends on the prognosis (prediction of whether the tooth can be saved or not) and you still have to keep your oral hygiene good at all times.
For bruxism cases, wearing a mouth guard/splint at night might be useful to reduce the symptoms. As the habit has always been related to stress, it is advisable for the bruxist to relax and get a good night’s sleep. Muscle relaxation exercises may also help in such cases.
Prevention
It goes without saying that prevention is better than cure. Maintenance of good oral hygiene is the key element to avoid periodontal disease. It can be achieved by brushing efficiently, at least three times a day, avoiding biting or chewing on hard food, eating healthy diet, and having a routine dental check-up six monthly.
In a nutshell, when the tooth feels loose, don’t take it for granted! Please see your dentist immediately. The most important thing here is to stop the progression of the disease. Loose does not mean to be lost! Early treatment will help you to save your teeth! Don’t forget to request for the gum screening during the visit as it is a different procedure than ordinary dental check-up
References
- Clinical Periodontology and Implant Dentistry,Sixth Edition,Jan Lindhe, Niklaus P. Lang, Thorkild Karring
- http://dentalmobility.com/en/tooth-mobility.html
- http://www.dentalcare.com
- http://en.wikipedia.org/wiki/Tooth_mobility
- http://www.nidcr.nih.gov/oralhealth/Topics/GumDiseases
- http://www.nhs.uk/Conditions/teeth-grinding
| Last Reviewed | : | 19 June 2015 |
| Writer | : | Dr. Rusmizan bin Yahaya |
| Accreditor | : | Dr. Rasidah bt. Ayob |