Introduction
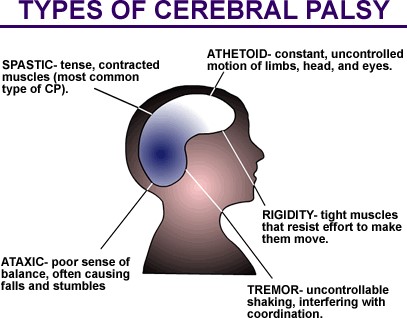
Cerebral palsy is considered a neurological disorder caused by a non-progressive brain injury or malformation that occurs while the child’s brain is under development. Cerebral palsy primarily affects body movement and muscle coordination. Though cerebral palsy can be defined, having cerebral palsy does not define the person that has the condition. Current research suggests the majority of cerebral palsy cases result from abnormal brain development or brain injury prior to birth or during labour and delivery. Accidents, abuse, medical malpractice, negligence, infections, and injury are some known risk factors that may lead to cerebral palsy.
 |
| Resource : http://stemcelltreatments.in/yahoo_site_admin/assets/images/CP.47160630_std.gif |
Diagnosis
- Developmental history.
- Physical examination with careful attention to growth patterns, dysmorphic features and skin stigmata of neurocutaneous disease, and thorough neurologic examination.
- Clinical diagnosis of cerebral palsy is based on the pattern of abnormalities on neurologic examination:-
P – Abnormal Posture: fisting with adducted thumbs, hyperextension and adduction (scissoring) of lower extremities, and hyperextension of trunk (arching).
O – Poor Oral-motor coordination: poor sucking-swallow coordination, poor lip closure on the nipple, difficulty handling textured foods, or excessive drooling. Older kids may have trouble with drooling, chewing or articulation.
S – Strabismus: abnormal alignment of the eyes, commonly associated with cerebral palsy.
T – Abnormal muscle Tone: increased resistance to passive movement of the extremities and decreased axial tone.
E – Delayed integration of primitive reflexes, delayed Evolution of automatic responses: persistent palmar grasp, Moro, asymmetric tonic neck reflexes. Poor equilibrium, delayed protective response.
R – Deep tendon Reflexes: brisk, with clonus.
* Infants with 4 or more of these findings are likely to receive the diagnosis of Cerebral Palsy
later in childhood.
Effect of Cerebral Palsy
- Cerebral palsy affects body movement, muscle control, muscle coordination, muscle tone, reflex, posture and balance. It can also impact fine motor skills, gross motor skills and oral motor functioning.
- Those with cerebral palsy may have only minor difficulty with fine motor skills, such as grasping and manipulating items with their hands.
- A severe form of cerebral palsy could involve significant muscle problems in all four limbs, mental retardation, seizures, and difficulties with vision, speech, and hearing.
- Muscles that receive defective messages from the brain may be constantly contracted and tight (spastic), exhibit involuntary writhing movements (athetosis), or have difficulty with voluntary movement (dyskinesia).
- There can also be a lack of balance and coordination with unsteady movements (ataxia)
- Effects on the muscles can range from mild weakness or partial paralysis (paresis), to complete loss of voluntary control of a muscle or group of muscles (plegia).
Cerebral palsy is also designated by the number of limbs :-
- Monoplegia is one single limb being affected
- Diplegia is both arms or both legs being affected ,
- Hemiplegia is both limbs on one side of the body being affected.
- Quadriplegia is all four limbs being affected.
How physiotherapy can help?
Physiotherapy plays a central role in managing the condition, often from birth. After problem is identified, physiotherapist will assess the child and record their development. As part of a tailored treatment plan we will teach the child how to control their head movements and how to sit, roll over, crawl and walk, as well as trying to inhibit abnormal reflexes and patterns of movement as well as teaching and guiding the parent.
Although it is a lifelong disability, much can be done to reduce the impact of cerebral palsy.
It is important for children to receive support from an early age to ensure they have every opportunity to reach their full potential.
- Passive stretching exercises to prevent muscles shortening and losing their normal range of movement.
 |
 |
To stretch the muscles, the arms and legs must be moved in ways that produce a slow, steady pull on the muscles to keep them loose.
Do it one joint at a time. Always protect the joint and move gentle but firm. Move 10 repetitions and hold for 30 second each repetition.
The effect of stretching depends on tension applied to the soft tissue, duration, repetition in session, and daily frequency. Slowly sustained stretch managed painful contractures.
- Balance training in sitting and standing
 |
 |
 |
| Sitting on medicine ball | Half kneeling | Stand upright for 1 minute without holding on. |
3. Upper limb activity
 |
 |
| Train patient to do active exercises for upper limb in sitting position without support. | Patient sits in the corner chair. |
Effective use of the upper limb can impact on educational outcomes, participation in activities of daily living and vocational options for many children with cerebral palsy. Making exercises as functional as possible will make it easier for them to be incorporated into daily life.
The role of parents and support measures that can be done at home
1.Exercises with the child regularly
Exercises with A child can maintain/improve the skills gained during therapy if the skills are practiced regularly during their daily life. Making exercises as functional as possible will make it easier for them to be incorporated into daily life.
2. Mobility
Many children cerebral palsy will experience difficulty moving around in their environment. This can range from problems turning over in bed to not being able to move on the floor or difficulties with walking. The child may need more time to get around, or need to use a walking aid or a wheelchair. As the child becomes older, adaptations to the house may become necessary.
3. Make sure activities include able-bodied children and adults.
It’s great to participate in activities that include other children with disabilities because it helps children realize that they’re not alone. But as they grow up, more able-bodied people will enter their world.
4. Encourage a child to share his or her story
A child with a disability may not feel comfortable talking about the nature of his or her disability. And, there may be subjects they may never speak about. But sharing how or why they have a disability, and showing that they are capable of speaking and relating to other children, shows everyone that a person who has disabilities is more like everyone else than different.
Prognosis
- The majority of children survive into adulthood, with a 30 year survival rate of about 87%.
- Motor impairment is variable among the different subtypes of cerebral palsy, but studies have helped improve prognostication in this regard.
References
- Kuban K.C. and Leviton A. Medical Progress: Cerebral Palsy. NEJM 1994
- Kinsman S.L. Predicting gross motor function in cerebral palsy. JAMA 2002
- Palmer F.B. Strategies for the early diagnosis of Cerebral Palsy. The Journal of Pediatrics August 2004
- R. L. Braddom, Physical Medicine and Rehabilitation, WB Saunders, Philadelphia, Pa, USA, 2nd edition, 2000.
- K. H. Tsai, C. Y. Yeh, H. Y. Chang, and J. J. Chen, “Effects of a single session of prolonged muscle stretch on spastic muscle of stroke patients,” Proceedings of the National Science Council, Republic of China B, vol. 25, no. 2, pp. 76–81, 2001
- http://www.childsplayphysio.com.au/
- http://cerebralpalsy.org/information/acceptance/tips-for-parents
Source image
- http://stemcelltreatments.in/yahoo_site_admin/assets/images/CP.47160630_std.gif
- Unit Fisioterapi, Hospital Melaka
| Last Reviewed | : | 23 August 2019 |
| Writer / Translator | : | Ismawi bin Ismail |
| Accreditor / Reviewer | : | Halimah bt. Hashim |







