What is Terminal Illness? What is this particular terminal disease?
Terminal illness is an incurable disease and there is no cure, and death cannot be avoided in the time varying according to the potential of the patient (Stuard & Sundeen, 1995). Considered the terminal disease patients have no hope of recovery and are waiting death any time. Examples of terminal diseases include AIDS and cancer.
Terminal Illness Criteria
- The disease cannot be cured
- Leads to death
- The medical diagnosis is unclear
- There is no medicine to cure
- The prognosis is negative
- Being progressive
The Terminal Patient Will Suffer Loss Consists of Two Forms :
a) Loss of real (actual loss) the loss of a person or object is no longer felt, seen, touched. For example: loss of limbs, roles, relationships.
b) The loss is felt (perceived loss) and it is natural that will causing distress. For example: loss of self-esteem, confidence.
Examples of Losses
- Loss of objects
- Loss of neighbourhood known
- Loss of something or someone very important and meaningful
- Loss of an aspect of themselves
- Loss of life / direction
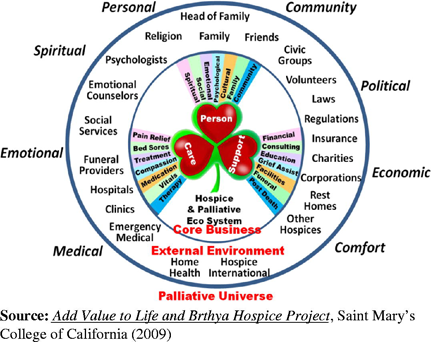
Table 1 : Values of Life in Hospice & Palliative Eco System
Understanding Changes
1. Grieve (grieving) – an emotional reaction to loss. Grieving manifested in many ways unique to the individual and based on personal experiences, different cultures, spiritual beliefs and practices.
2. Mourning – is the time of acceptance of loss and grief. Mourning of the loss occurred in the past and also often influenced by culture or customs.
Patients Understand Changes
According to “Lindermann” in his study have expressed feelings of grief not only emotional, but it also involves physical, cognitive, behavioral and emotional of the patient.
Physical Sensation Changes
• Stomach twisting / hollowness in the stomach
• Tension in the chest / tightness in the chest
• Tension in the neck / tightness in the throat
• Sensitive to noise / oversensitivity to noise
• Feeling alienated / A sense of depersonalization
• Difficulty breathing / breathlessness, feeling short of breath
• Muscle pain / weakness in the muscles
• Lack of power / lack of energy
• Dry mouth
Cognitive Changes
• feelings of not believing / disbelief
• confused
• fill your time with activities / preoccupation
• significant feeling of awareness / sense of presence
• hallucinations
Behavioural
• Sleep disturbance
• Disruption of appetite
• Negative behavior / absentminded behavior
• Personal separation/ Social Withdrawal
• Want to die
• Crying
Grieving Reactions
Terminal patients will experience a level of grief response. According to Kubler – Ross, grieving stage comprises :
a) Denial,
b) Rage / Anger,
c) Bargaining
d) Depression
e) Acceptance
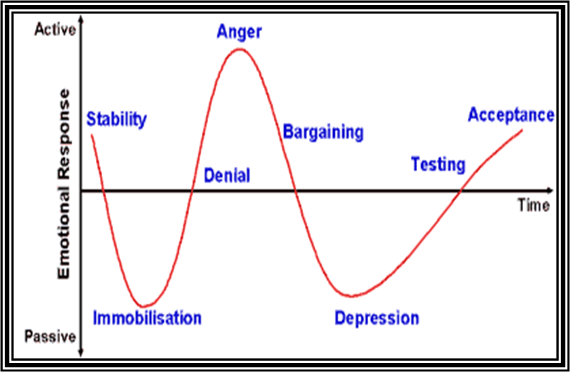
Table 2 : Current Responses Emotional Graf Individual A Grieving
1. Refusal / Denial
• Denial is the first reaction upon receiving news of the patient’s condition.
• Cognitive changes are as non-believers, understand, or do not accept.
• The physical changes are fatigue, weakness, paleness, nausea, crying, respiratory and nervous disorders.
• The length of time lasting a few minutes to a few years.
• Example – “I feel ok, I have no problem.”; “No, these things would not happen inside of me!”
2. Anger
• Patients may experience anger terminal.
• Anger arises and it is projected towards others or him.
• Physical changes are patient will be aggressive, rude speech, attacking others and refusing treatment.
• Behavioral of the patients will also change, these patients also were outraged and accused the doctor or nurse is not competent and professional in their work.
• The patient will experience flushing, rapid pulse, anxiety, insomnia and trembling hands
• Example – “Why me? This is not fair!”; “Why does this happen at me!”; “Whose fault is that?”
3. Bargaining – Offer
• The process of reality unpensioning to a loss of consciousness.
• It tries to bargain – bargain with the mercy of the Creator.
• Examples “share my life a little longer to see my big brother.”; “I’ll do anything as long as I can blow a bit longer.”; “I’m going to my savings if …”
4. Depression
• These patients demonstrate a retreat
• Patients are sometimes behave in accordance with, do not want to talk, unable to make decisions and think she is unworthy.
• The patient has suicidal thoughts.
• Physical symptoms are loss of appetite, feeling restless sleep, fatigue and decreased libido
• Examples “I feel sad matter, why do we bother me any more about?”; “I’ll be dead soon …… why should I …?”; “I really miss him, why should I live longer?”
5. Acceptance
Thoughts about lost things will start to diminish or disappear on switch to something new.
• Family members can accept the loss and start to look forward.
• When this positive environment is reached, the patient will accept the positive feelings and cope with feelings of loss or negative.
• Examples “I’ll be fine.”; “I was able to tackle it and will change”; “I cannot fight, but I’d be willing je!”Mental
Preparation of the Caregiver
Caring for the sick is not easy. Guardian (caregiver) be prepared emotionally, mentally and physically. Thus, the guardians had to build and enhance relationships of trust with:• Listen to the patient speaks.
• Provide encouragement to the patient she/he is willing to express his feelings.
• Answering patient’s question directly.
• Show acceptance and empathy.
• Provide support to patients lost response.
• Increase the sense of togetherness among family members.
• Determine the patient’s illness level.
Terminal Patient Identification Requirements
Health workers and guardians / parents must identify the emotional needs of patients with terminal for their understanding.
Denial
• Provide an opportunity to express feelings of terminal patients
• Show acceptance with sincere attitude and encourage patients to express themselves.
• Give honest answers to the questions the patient about his illness.
Angry
• Allow and encourage patients to express their anger verbally, without provoking anger. Keep in accordance with cultural and religious restrictions.
• Family members should be explained that the anger that do not actually addressed to them.
• Family members should let the patient cry and encourage the patient to discuss about his anger.
• Family members should help patients with :
- Listen attentively.
- Encourage the patient to talk about fear or guilt.
- If the patient always expresses “when” or “if only ….”tell patients that the health worker can only do something real.
- Tell patients about the cause of guilt and fear.
Level Depression
• Help patients identify guilt and fear to observe the behavior of patients and explore her feelings with him.
• To help patients reduce guilt to avoid any action hurting yourself :
- Respect the feelings of the patient.
- Helping patients find a positive mind to give good release.
- Allowing the patient to express feelings and negative thoughts immersing patients with recurrent.
The Level of Acceptance
• Helps patients who do not accept the loss cannot be avoided :
- Assisting family members to visit the patient regularly.
- Assist the family so they do not mourn.
- Provide information about the patient’s family members.
Support Groups: NGO’s
The following are support groups or NGOs in Malaysia and abroad:
Ranking Malaysia
• Ministry of Health Malaysia (http://www.moh.gov.my/)
• National Cancer Society of Malaysia (NCSM) (http://www.cancer.org.my/index.php)
• Hospice Malaysia (www.hospismalaysia.org)
• Malaysian Oncological Society (http://www.malaysiaoncology.org/)
• Malaysian Medical Association (http://www.mma.org.my/)
• Breast Cancer Welfare Association Malaysia (http://www.radiologymalaysia.org/breasthealth/bcwaindex.htm)
• College of Radiology, Academy of Medicine of Malaysia (http://www.radiologymalaysia.org/)
World Rankings
• World Health Organization (WHO) (http://www.who.int/en/)
• International Association for Hospice and Palliative Care (IAHPC) (http://hospicecare.com/home/)
• Asia Pacific Hospice Palliative Care Network (PHN) (http://aphn.org/)
• Hospicenet (http://www.hospicenet.org/)
• Palliative Care Network (http://www.palliativecarenetwork.com/)
• National Hospice and Palliative Care Organization (NHPCO) (http://www.nhpco.org/)
• National Council for Palliative Care (NCPC) (http://www.ncpc.org.uk/)
• Singapore Hospice Council (http://www.singaporehospice.org.sg/)
| Last Reviewed | : | 24 February 2014 |
| Writer | : | Lee Boon Hock |
| Translator | : | Lee Boon Hock |
| Accreditor | : | Tn Hj Hairol Kamal bin Abdul Rahman |







