Introduction
All diseases related to abnormal function of an artery (vessels that bring oxygen to the body) can be classified under a disease known as Macrovascular disease (disease of the large artery – like artery to the heart called coronary artery and to the brain is cerebrovascular).
Cerebrovascular complications make diabetic patients two to six times more susceptible to a stroke event and this risk is magnified in :
-
older individuals, and
-
patients with hypertension. 4
What is ‘Cerebrovascular Disease’ ? 4
Cerebrovascular disease is any disease by which the arteries in the brain, or are connected to the brain, are DEFECTIVE.
The central mechanism in macrovascular disease is the process of atherosclerosis (walls of the blood vessels become thickened and hardened), which leads to narrowing of arterial walls throughout the body.
A stroke occurs when the blood flow to part of the brain is cut off – it is a ‘brain attack’ (in the same way that a heart attack happens when the blood supply to the heart muscle is cut off). Without a blood supply, brain cells can be damaged or destroyed because they may not receive enough oxygen.
Stroke can affect many different body functions, depending on the part of the brain that is involved.
What Are The Types of Stroke ? 3
There are two main types of stroke.
-
The most common type (an ischaemic stroke) is when one of the blood vessels leading to or in the brain is blocked either by thrombosis or embolic.
-
The second type (haemorrhagic stroke) is when a blood vessel in the brain bursts, causing bleeding into the brain.
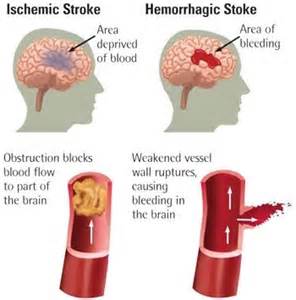
Figure 1: Ischaemic and haemorrhagic stroke.
(source : http://floydmemorial.com/healthscope/understanding-stroke-the-basics/)
A Transient Ischaemic Attack (TIA), often called a ‘mini-stroke’, happens when the blood supply to part of the brain is interrupted for a short time.
The symptoms are the same as for a stroke, but they usually last only a few minutes or hours, and disappear altogether within 24 hours.
Signs and Symptoms of Cerebrovascular Disease
The signs and symptoms of cerebrovascular disease depend on the location of the :
-
hemorrhage,
-
thrombus, or embolus, and
-
extent of brain tissue affected.
General signs and symptoms of a hemorrhagic or ischemic event include motor dysfunction, such as hemiplegia and hemiparesis. Patient may also presented with ;
-
vomiting,
-
seizures,
-
confusion
that leads to a ;
-
complete loss of consciousness,
-
labored or irregular respirations,
-
apneic periods,
-
increased blood pressure, and
-
bowel and bladder incontinence.
Patient may lose gag reflex and ability to cough and swallow leading to dysphagia. Patient may have communication deficits, such as dysphasia, receptive or expressive aphasia, dysarthria, and apraxia.
Signs and symptoms specific to a hemorrhagic cerebrovascular accident (CVA) include abrupt onset of a severe headache, nuchal rigidity, and rapid onset of complete hemiplegia. As the hematoma enlarges, the patient’s neurologic deficits worsen from gradual loss of consciousness to coma.
Symptoms of a thrombotic CVA follow the “stroke in evolution” pattern and include the progressive deterioration of motor and sensory function, slow deterioration of speech, and lethargy. These signs and symptoms peak when edema develops, usually about 72 hours after the onset of the thrombotic event.
For a patient with an embolic CVA, signs and symptoms include a sudden onset of motor and sensory deficits, deteriorated speech, and headache on the side of the head where the embolism is occurring. If the embolus breaks into smaller pieces and the occlusion resolves, these signs and symptoms may dissipate.
Following these, some individuals may experience stress and depression.
* CVA = Cerebrovascular Accident = Stroke (permanent loss of brain function) = TIA (temporary loss of brain function)
What Are The Risk Factors ? 4
People who suffer from strokes have often experienced other health problems in their life. These are called vascular risk factors because if a person has experienced one of these it increases the risk of them having a stroke or developing Cerebrovascular Disease.
-
High blood pressure : The most common risk factor
-
Diabetes mellitus
-
High cholesterol level
-
Heart disease
-
Smoking
-
High level of alcohol consumption
How To Make Diagnosis ?
Physical examination by a doctor looking for specific neurological, motor and sensory deficits such as ;
-
changes in vision or visual fields,
-
abnormal reflexes,
-
abnormal eye movements,
-
muscle weakness,
-
decreased sensation, and
-
other changes.
A computed tomography (CT) scan is used to diagnose and detect hemorrhagic strokes, since blood, bone and brain tissue can be easily distinguished due to their difference in densities. It is important to note that damage from ischemic stroke CANNOT BE DETECTED by this scanning method.
Patients with clinical evidence of stroke, may need an early brain CT scan because :
-
They may benefit from treatment to dissolve a blood clot (‘thrombolysis’) or reduce blood clotting.
-
They were taking drugs to reduce blood clotting (anticoagulants) before the stroke.
-
They are prone to bleeding.
-
They are unconscious.
-
Their symptoms are varying or getting worse for no obvious reason.
-
They have increased pressure at the back of their eyes (called ‘papilloedema’), a stiff neck or fever.
-
They had a very bad headache when the stroke symptoms began.
Is There Any Treatment ? 6
Aspirin should usually be given to people who have had an ischaemic stroke or other antiplatelet if contraindicated. These drugs have been effective in treating patients with a history of stroke or patients at risk for a stroke event.
Normally a person who has had a stroke shouldn’t be given anticoagulants (drugs to reduce blood clotting) unless there is a particular reason for this.
A drug to dissolve blood clot may be given if the person’s brain scan indicates that it might be helpful.
Nutrition and Swallowing Problems
People often have difficulty swallowing after having a stroke. In some cases, this can lead to problems such as pneumonia. Before a person who has had a stroke is given any food, liquid (including water) or medication by mouth, their swallowing should be checked by a trained healthcare professional.
If someone is unable to swallow, they should be given food and fluids through a tube that is passed through their nose into their stomach. This should happen within 24 hours of being admitted to hospital.
Medication should also be given by tube or suppository.
Anyone who is in hospital after a stroke should be screened when they are admitted and then once a week to make sure that they are not malnourished (body not received enough nutrition). If necessary, the person should be offered nutritional supplements, feeding through a tube and/or specialist dietary advice.
Blood Sugar
The healthcare team should make sure that the person’s blood sugar is within the normal range. If they have diabetes, they may need insulin injections and glucose.
Blood Pressure
Treatment to lower blood pressure should be given only if a person’s blood pressure is very high and they have another serious medical condition. High blood pressure may also be treated if a person is to be given thrombolysis.
Moving About
Anyone who has had a stroke should be helped to sit up in bed, and to get out of bed and move around the stroke unit, as soon as they are able to.
Stroke Rehabilitation
Rehabilitation is a very important component in overall management of stroke patient and it should be started from admission in the ward. Family or carers commitment play an important role in making the rehabilitation to be successful.
References :
-
http://www.nice.org.uk/nicemedia/live/12018/41315/41315.pdf (accessed on 19 September 2012)
-
http://clinical.diabetesjournals.org/content/26/2/77.full
-
http://www.diabetesdaily.com/wiki/Cerebrovascular_disease
-
http://www.cerebralfunctionunit.co.uk/CVDinfosheet.html
-
http://www.bing.com/images/search?q=Hemorrhagic+Stroke&FORM (accessed on 20 September 2012)
-
Ministry of Health Malaysia: CPG Ischaemic Stroke 2000
-
http://www.medterms.com/script/main/art.
| Last reviewed | : | 20 January 2014 |
| Writer | : | Dr. Hamimah Saad |







