Monitoring of Complications
Introduction
The eye is an important organ that allows vision. Retina is part of the eye that consists of a number of cells and normal vision depends on intact-cell communication among them.
Diabetes and chronic exposure to hyperglycaemia (high glucose in the blood) damages all the major retinal cells of the retina and cells of the blood vessels. [1, 2].
Diabetes induces damages to the retinal cells. The extent of damages correlates with excessive circulating levels of glucose, lipids, hormones, amino acids and inflammatory molecules [3].
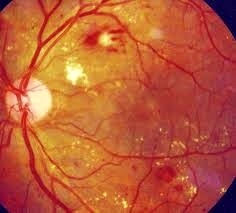
The diagram below shows an example of the damaged retinal cells. Abnormality in the retina caused by diabetes complication is referred to as diabetic retinopathy.
 |
 |
Diagram 1 : Non-Proliferative Diabetes Retinopathy [7]
Eye Examination
Eye examination is mandatory in diabetes patients to detect changes and damages to the retina. Visual acuity (ability to read a vision chart (Snellen chart) at a distance) and funduscopy (examination of the retina using a funduscopy) are 2 ways of doing eye examination in diabetes patients.
Abnormality in any of the test renders further assessment by a specialist.
- VISUAL ACUITY
- This is a test which uses an eye chart to measure how well a person sees at various distances.
- FUNDUSCOPY
- This is an examination of the eyes using a hand held ophthalmoscopy. The eyes can also be examined using a fundus photography which enables one to examine larger areas of the retina. It has an advantage of photo documentation for future references.
Why The Need To Do Eye Examination?
Diabetic retinopathy (retinal damages due to diabetes) is one of the microvascular complications (abnormality of the small blood vessels) of diabetes.
Diabetes Control and Complications Trial (DCCT) [3] and the UK Prospective Diabetes Study (UKPDS) [4] have established that hyperglycaemia is the initiating cause of retinal damage.
If diabetic retinopathy is not managed appropriately, it will lead to blindness.. It affects up to 80% of diabetes patients of more than ten years duration [1].
When To Screen For Diabetic Retinopathy
Diabetic retinopathy has no early warning signs. Screening for diabetic retinopathy should be done upon diagnosis for type 2 diabetes mellitus and at five years for type 1 diabetes mellitus [6].
Screening should not be delayed if patients experience changes in their vision. Referral to eye specialist is needed when indicated.
Measures To Be Taken To Prevent Diabetic Retinopathy
- Optimal control of diabetes
- Treat hypertension to target
- Control of dyslipidaemia (abnormality of cholesterol and fat profiles)
- Yearly screening for diabetic retinopathy
- Smoking cessation
Below is a diagram showing the retina after treating it with laser therapy. Laser therapy is one of the treatment options for diabetic retinopathy.
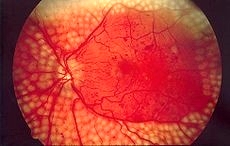
Diagram 2 : Retina after laser therapy [7]
Conclusion
Eye examination in a diabetes patient should be done annually. It is essential in detecting early diabetes retinopathy. Management must focus on achieving optimal glucose control and related co-morbidities.
References :
- Mizutani M, Kern TS, Lorenzi M. Accelerated death of retinal microvascular cells in human and experimental diabetic retinopathy. J. Clin. Invest. 1996; 97(12) : 2883-90.
- Hammes HP, Strodter D, Weiss A, Bretzel RG, Federlin K, Brownlee M. Secondary intervention with aminoguanidine retards the progression of diabetic retinopathy in the rat model. Diabetologia 1995; 38(6) : 656-60 (1995).
- Ahmed M. Abu El-Asrar,; Hani S. Al-Mezaine,, Mohammad Shamsul Ola. Pathophysiology and Management of Diabetic Retinopathy: Pathophysiology of Diabetic Retinopathy. Expert Review of Ophthalmology 2009; 4(6): 627-47.
- Wong TY, Liew G, Tapp RJ et al.. “Lancet Revision, D-07-06757 The Relationship of Fasting Glucose to Retinopathy: Re-visiting a Key Criterion Used to Diagnose Diabetes”. Lancet 2008 ; 371 (9614): 736–43.
- Williams R, Airey M, Baxter H, Forrester J, Kennedy-Martin T, Girach A “Epidemiology of diabetic retinopathy and macular oedema: a systematic review”. Eye 2004; 18 (10): 963–83.
- Malaysian Clinical Practice Guideline on Management of Type 2 Diabetes Mellitus 2009.
- http://en.wikipedia.org/wiki/Diabetic_retinopathy –accessed 20th September 2012.
- http://www.google.com.my/search?q=diabetic+retinopathy+pathophysiology – accessed 20th September 2012.
| Last reviewed | : | 13 January 2014 |
| Writer | : | Dr. Sri Wahyu binti Taher |







