Wilms’ tumour is a solid tumour of the kidney that arises from immature kidney cells. It is the most common primary malignant renal tumor in children and the fourth most common type of cancer in children .It was named after Dr Max Wilms, who first described it in 1899.Wilms’ tumours usually only affect one kidney (unilateral) but in about 7 out of every 100 children it can affect both (bilateral).
When a baby is growing in the womb, there are special cells called metanephric blastema that is involved in the development of the child’s kidneys. These cells normally disapper at birth but in some children these cells may persist. Wilm’s tumour is thought to grow out of these metanephric blastema.
The Kidneys
The kidneys are a pair of organs found at the back of the abdomen. They filter the blood by removing waste products such as urea and salt, and water which are then passed to the urinary bladder where they leave the body in the form of urine.
Epidemiology
The annual incidence rate of Wilms’ tumor is about 7-10% cases per million of 15 years. This account for 6-7% of all childhood cancers. Wilm’s tumour almost exclusively in children. Majority are diagnosed before 5 years of age with a median age of 3.5 years.
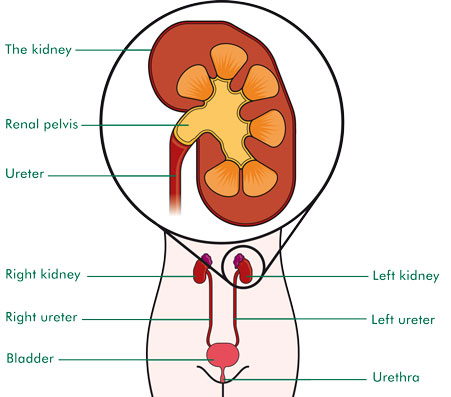
Structure of the kidney
Causes
In most cases, the cause of Wilms’ tumour is unknown. However, it is believed to occur as a result of changes in 1 or more genes. Several types of birth defects or congenital anomalise appear to be associated with the occurrence of Wilm’s tumour. Children with these anomalies should be screened regularly for Wilm’s. About 15 out of every 100 children who develop a Wilms’ tumour also have a birth defect.
Most birth defects associated with Wilms’ tumours happen in syndromes. A syndrome is a group of symptoms and abnormalities that are present in the same person. Gene mutations affect all body cells. So this explains why children born with one of these syndromes can have several parts of their body affected and not just their kidneys.
The main ones are:
- WAGR syndrome is a combination of abnormalities in the coloured part of the eye (iris), the genitourinary tract and the brain. The person may have learning disability.
- Beckwith-Wiedemann Syndrome means that children have larger than normal internal organs and often have a big tongue. One side of the body maybe slightly larger than the other.
- Denys-Drash Syndrome means that babies have under development of the penis, scrotum or testicles and can be mistaken for girls. The kidney function is affected and Wilms’ tumour may develop in the damaged kidney.
In addition 1 in 100 people with Wilms’ tumour may have a family member with Wilms tumour . These patients usually presented early and has an increased risk of bilateral disease.
Signs and Symptoms
- Painless abdominal/ tummy swelling -the commonest presentation
- usually noted by mother during bathing the child.
- Bleeding inside the tumour causing abdominal pain
- Blood in the urine – found in between 15 and 20 out of every 100 children (15 to 20%) with a Wilms’ tumour
- Raised blood pressure
- High temperature (fever)
- Loss of appetite
- Weight loss
- Feeling or being sick
- Shortness of breath and cough (if the cancer has spread to the lungs)
How Wilms Tumour is diagnosed?
The doctor will carry out a physical examination. If Wilm’s tumor is suspected, several investigations will be performed. These include :
- Blood tests
Blood tests are used to check a child’s general health (especially before surgery) . These may include tests that look at the number of white blood cells, red blood cells, and platelets, and tests to measure the function of the liver and kidneys. - Urine
A urine sample may be tested (urinalysis) to look for blood and other substances in the urine that might suggestive of kidney problem. - Radiology / imaging
- Ultrasound and Doppler sudy
This is often the first imaging test done if the doctor suspects your child has a Wilms tumor because it is easily available and no radiation .It gives the doctor a good view of the kidneys and the other organs in the abdomen. The Doppler can be used to evaluate the tumour extension to the adjacent vessel. The test is not usually painful, but it might cause some discomfort if the transducer is pressed down hard on the abdomen. - CT scan/CAT scan – Computed tomography scan
A CT scan is a special x ray and one of the most useful tests to look for a mass inside the kidney. It is also helpful in checking whether a cancer has spread to organs and tissues beyond the kidney, such as the lungs and liver. - Magnetic resonance imaging (MRI) scan
Uses radio waves and strong magnets to produce detailed pictures of the internal parts of the body. This provide more intricate images that allow doctors to see if th cancer has invaded any major blood vessels near the kidney. May not be necessary if CT scan has already provided the information required.
- Ultrasound and Doppler sudy
- Chest x-ray
Chest x-rays may be done to look for any spread of Wilms tumor to the lungs, as well as to have a baseline view of the lungs to compare with other x-rays that might be done in the future. If a CT scan of the chest is done, this test is not needed but might required during follow up. - Kidney biopsy/surgery
- Surgery
Most of the time, imaging tests can give doctors enough information to decide if a child probably has a Wilms tumour, and therefore surgery should be done. But the actual diagnosis of Wilms tumour is made when a sample of the tumour is removed and looked at under a microscope. This is call histology
In most cases, the sample is obtained during surgery to treat the tumour.
The central line called porta-cath or Hickman line will also be inserted at the chest during the surgery under general anaesthesia. This line is important for chemotherapy administration and blood taking. - Biopsy
Sometimes if the doctors are less certain about the diagnosis or if they are not sure the tumour can be removed completely, a sample of the tumour may be obtained first. The biopsy may be done either surgically or using a long, hollow needle that is inserted through the skin and into the tumour.
- Surgery
- Other Investigations
- Echocardiography
This investigation is similar to an ultrasound except that it specifically look at the heart structure and function prior to chemotherapy . One of the chemotherapy drugs used to treat wilm’s tumour has an effect on the function of the heart - Bone scan
Bone scan will be done if the cancer is suspected to have spread to the bones.
- Echocardiography
Staging of Wilms Tumour
The stage of a cancer is a term used to describe its size and whether it has spread beyond its original site. Knowing the stage of the cancer helps doctors decide on the most appropriate treatment.
A commonly-used staging system for Wilms’ tumour is described below.
Stage 1
The tumour is confined to the kidney and has not begun to spread. It can be completely removed with surgery.
Stage 2
The tumour has begun to spread beyond the kidney to nearby structures such as surrounding fatty tissue, but it’s still possible to remove it completely with surgery. No lymph node involvement
Stage 3
The tumour has spread beyond the kidney; either because the tumour has burst before (or during) the operation, has spread to lymph node or has not been completely removed by surgery.
Stage 4
The tumour has spread to other parts of the body such as the lungs, liver, bones and brain. Tumours in other parts of the body are known as metastases.
Stage 5
There are tumours in both kidneys (bilateral Wilms’ tumour).
If the tumour comes back after initial treatment, this is known as recurrent cancer or relapse.
Treatment
Children with cancer should be treated at specialised centres which are familiar with the management of paediatric caners. The treatment involves a multidisciplinary team which include the paediatric oncologist, paediatric surgeon, paediatric radiologist and radiotherapist as well as pathologist, medical social worker and dietitian.
Treatment will depend on a number of factors including how the cells appear under the microscope (histology) and the stage of the tumour. Treatment includes surgery, chemotherapy and/ or radiotherapy.
- Surgery
All children with Wilms’ tumour will need to undergo surgery either upfront or after a few cycles of chemotherapy. The operation usually involves removing the whole of the affected kidney (nephrectomy). - Chemotherapy
Chemotherapy is the use of anti-cancer (cytotoxic) drugs to destroy cancer cells. It’s usually given as an injection or drip into a vein (intravenously). Chemotherapy given before surgery is called neoadjuvant chemotherapy.
The number, type and duration of the chemotherapy regiment will depend on the histology of the tumour and the stage of the disease. The paediatric oncologist will explain in detail the treatment as well as the potential side effects of the various drugs used. - Radiotherapy
Radiotherapy treats cancer by using high-energy rays to destroy the cancer cells, while doing as little harm as possible to normal cells.
Not all children with Wilms’ tumour need radiotherapy. Your child will be referred to Radiation Oncologist if he requires this modality of treatment
Treatment for bilateral Wilm’s tumour
In about 1 in 20 cases, Wilms’ tumour affects both kidneys. Treatment usually involves surgery to both. The aim of the treatment is to remove as much of the cancer as possible, while leaving as much healthy kidney as possible. Chemotherapy is always given. Sometimes radiotherapy is needed as well.
Side Effects of Treatment
Chemotherapy and radiotherapy carry a risk of side effects, which may be immediate or long-term.
Early
Side effects can include feeling sick (nausea) and being sick (vomiting) , hair loss, bruising and bleeding, tiredness, diarrhoea and an increased risk of infection.
Late side effects
A small number of children may develop late side effects.. These include a possible reduction in bone growth, a change in the way the heart and lungs work, and a slight increase in their risk of developing another cancer in later life. Infertility is a possible late side effect, although this is rare.
Prognosis
Improvement in the diagnosis and treatment of Wilm’s tumour has improved the outlook or prognosis of children with this disease. In general, the prognosis of this tumour is very good. The cure rate for Wilm’s tumour of good histology now exceeds 90%.
Treatment Centres Available in Malaysia
Need multidisciplinary care including Paediatric Oncologist, Pediatric Surgeon,.Peadiatric Radiologist/ Radiologist,. Radiation Oncologist,. Paediatric Cardiologist, Histopathologist, Medical social worker and Dietician.
- Klang Valley –
Paediatric Institute (MOH)
Pusat Perubatan Universiti Malaya – MOE
Pusat Perubatan Universiti Kebangsaan Malaysia- MOE
Sime Darby Medical Centre – Private - Northern States – Hospital Penang -MOH
- Perak – Hospital Ipoh – MOH
- Johor – Hospital Sultan Ismail – MOH
- Kelantan and Terengganu – Hospital Universiti Sains Malaysia – MOE
- Sabah – Women and Children Hospital – Likas – MOH
- Sarawak – Hospital Umum Kuching – MOH
| Last Reviewed | : | 18 November 2015 |
| Writer | : | Dr. Che Hadibiah bt. Che Mohd Razali |
| Accreditor | : | Dr. Eni Juraida bt. Abdul Rahman |







