Normally, we only hear about physical exercise. However, have you heard about face and mouth exercises? What is oral motor and its role in our daily life? This article will explain several aspects in oral motor.
Definition of Oral Motor
Oral motor refers to the structure and the function of the facial muscles (e.g. lips and jaw) and the oral cavity (e.g. tongue and soft palate).
Eating and speaking requires strength, coordination and control of oral structures.
Activity during eating includes:
- Sucking
- Biting
- Crashing
- Licking
- Chewing
Activity when speaking includes:
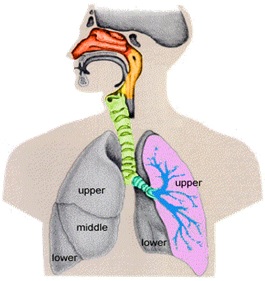
- Adequate air supply from the lungs for speaking (respiratory system)
- Frequency, strength and voice quality production (phonation system)
- Resonance sounds production such as nasal resonance (resonance system)
- Movement of articulators (lips, jaw, soft palate) to produce speech sounds (articulatory system)
- Intelligible speech that is easily understood
- Intonation, rhyme and rhythm production
Besides that, oral motor skills are also important for facial expressions.
Source: le.ac.uk
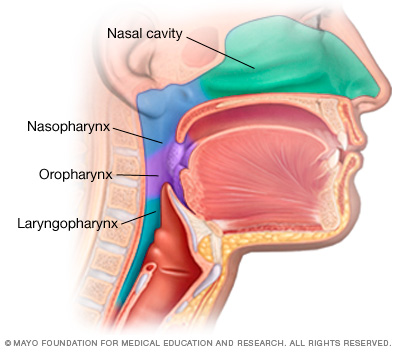
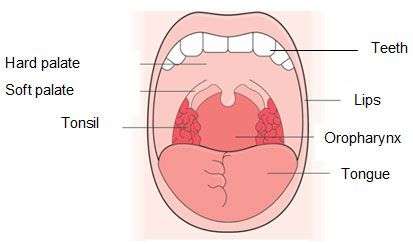
Structures and functions of the oral motor
It is important to understand the functions of the oral motor before carrying out any face and mouth exercises. The table below illustrates the structures and functions of the oral motor that is important for speaking and swallowing.
 |
 |
| Source: sparrow.org | Source: macmillan.org |
|
Structure |
Function |
Structure |
Function |
|
Lips |
|
Jaw |
|
|
Tongue |
|
Larynx |
|
|
Teeth |
|
Nasopharynx |
|
|
Hard palate |
|
Tonsil |
|
|
Soft palate |
|
Oropharynx |
|
What are the signs associated with oral motor problem?
Signs that can usually seen are as follows:
- Reduced strength and poor coordination of the lips, tongue and jaw
- Slurring of speech
- Drooling
- Weak facial musculatures
- Difficulty in chewing and swallowing
- Changes in voice quality
- Difficulty to make oral movement (mouth or tongue)
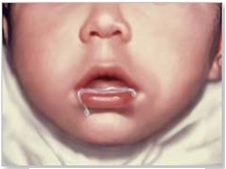
Drooling
Source: A.D.A.M
Who needs oral motor therapy?
-
Dysarthria (weakness, slowness and poor coordination in muscles that controls the movement of the speech due to damage/problems of the nervous system)
-
Apraxia (difficulty to plan, follow sounds in sequence and control the movement of the motor or muscles to produce speech. This problem is not caused by muscles problems/ weak nerves)
-
Structural defects (e.g. cleft lip/palate)
-
Down syndrome
-
Children who are diagnosed to have speech delay
-
Phonological or pronunciation problem (difficult to produce and form correct speech sounds)
Oral motor therapy approach
There are several oral motor approaches that can be applied. However, oral motor therapy is not the end solution to the speech and swallowing problem. Various studies on oral motor skills have been conducted and the outcomes showed that oral motor therapy alone is not helpful in terms of speech.
The techniques shown below are oral motor approach that is often used by Speech-Language Therapist (SLT):
- Mouth movement play
- Icing
- Horn tube
- Massage
- Vibration
- Oral motor play activity books
- Blowing bubbles
- Using mirror
- Video/ DVD recording
Oral motor therapy through oral facial and mouth play will be further explained in this article.
Oral motor therapy exercise
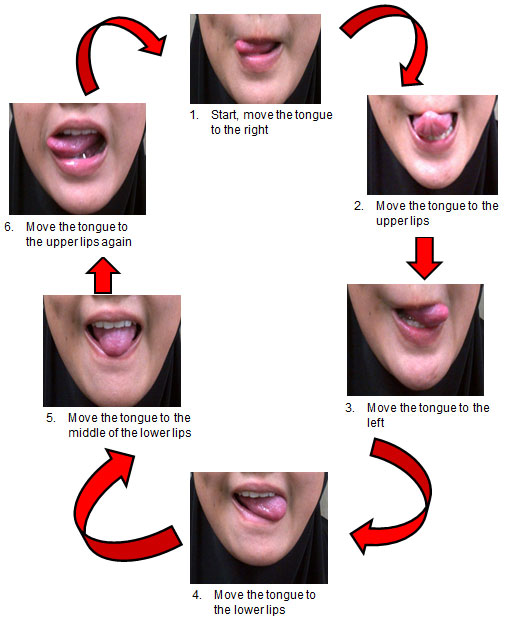
Exercise of the oral motor helps in increasing the strength, range of motion, and coordination of the lips, tongue and jaw. The diagram and the video below can be used as a guideline.
Oral Motor Therapy Diagram
-
Face
Tilt the face 
- Lips
Open and close the mouth 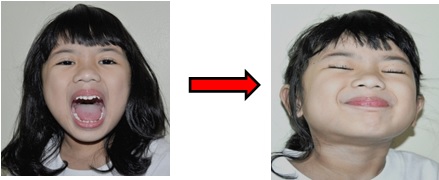
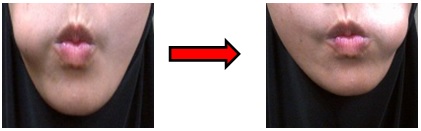
Opening Mouth Closing MouthPucker lips 
Puff the cheeks by holding the air and lips are sealed 
Smile, then relax the lips and cheeks 
Close the lips tightly, then open the mouth like the sound of “pop” 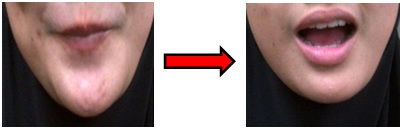
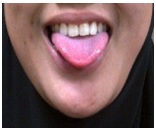
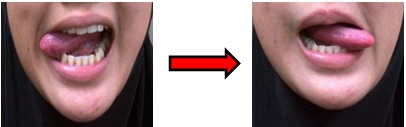
Close the lips tightly Open the mouth quickly,and let go the air - Tongue
-
Jaw
Open the mouth as wide as possible 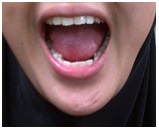
Slowly move the jaw to the right and left. Then move the jaw to the left and right as fast as possible. 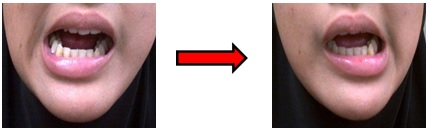
Move the jaw to the right Move the jaw to the left Slowly move the jaw up and down. Then move the jaw up and down as fast as possible. 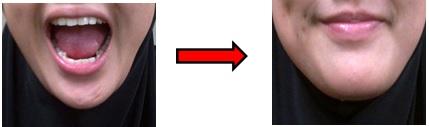
Move the jaw down Move the jaw up
The Effectiveness of Oral Motor Therapy
Oral motor therapy alone is not effective to help the clarity of speech. However, oral motor therapy can be applied to help the problems associated with:
- Activities during eating such as difficulty to move the tongue or chewing food
- Drooling of saliva which does not follow a normal developmental stage
Referrals
Oral motor problem can be identified depending on the children’s age and the stage of development.
Therefore, if there is a problem related to oral motor as described in this article, please refer to the following specialists:
- Pediatrician
- Dentist
- Orthodontist
- Prosthodontist
- Speech-Language Therapist
- Occupational Therapist
- Physiotherapist
- Sensory integration
References
- American Speech-Language-Hearing Association (ASHA). Speech-Language Pathology Medical Review Guidelines [PDF Document]. Retrieved from http://www.asha.org/uploadedFiles/SLP-Medical-Review-Guidelines.pdf
- Elamar. Oral Motor Exam Structures and Functions [PowerPoint slides]. Retrieved from Quizlet Online Website: http://quizlet.com/10524428/oral-motor-exam-structures-and-functions-flash-cards/
- Elamar. Oral Motor Development [PowerPoint slides]. Retrieved from Quizlet Online Website: http://quizlet.com/6580538/oral-motor-development-flash-cards/
- Hutton, T.L. Oral-Motor Workouts for Home [PDF Document]. Retrieved from Super Duper® Handy Handouts!® Online Website: http://www.superduperinc.com/handouts/pdf/179_Oral-MotorWorkout.pdf
- Kumin, L. Resource Guide to Oral Motor Skill Difficulties in Children with Down Syndrome [PDF Document]. Retrieved from Resource Guide Online Website: http://ndsccenter.org/worpsite/wp-content/uploads/2012/03/OralMotor.pdf
| Last Reviewed | : | 28 August 2020 |
| Writer / Translator | : | Nurshahira bt. Razali |
| Accreditor | : | Nur Fariha bt. Md. Shah |
| Reviewer | : | Nadwah bt. Onwi |