Definition
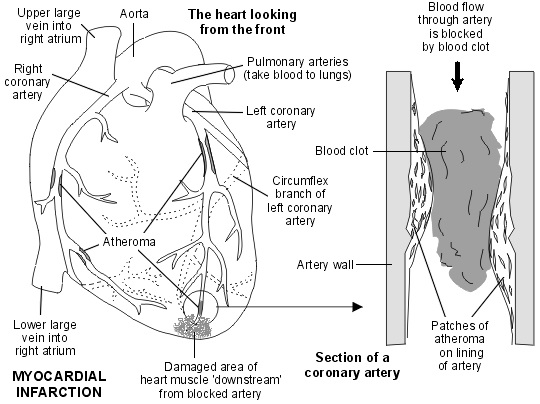
A heart attack (myocardial infarction) is usually caused by a blood clot, which stops the blood flowing to a part of the heart muscle.
What causes a myocardial infarction (MI)?
The most common cause of a myocardial infarction (MI) is a blood clot (thrombosis) that forms inside a coronary artery, or one of its branches. This blocks the blood flow to a part of the heart.
Blood clots do not usually form in normal arteries. However, a clot may form if there is some atheroma within the lining of the artery. Atheroma is like fatty patches or plaques that develop within the inside lining of arteries. Plaques of atheroma may gradually form over a number of years in one or more places in the coronary arteries. Each plaque has an outer firm shell with a soft inner fatty core.
What happens is that a crack develops in the outer shell of the atheroma plaque. This is called plaque rupture. This exposes the softer inner core of the plaque to blood. This can trigger the clotting mechanism in the blood to form a blood clot. (The diagram below shows four patches of atheroma as an example. However, atheroma may develop in any section of the coronary arteries.)
Subsequently the part of the heart muscle with blocked artery is at risk of dying unless the blockage is quickly removed. When a part of the heart muscle is damaged it is said to be infarcted. The term myocardial infarction (MI) means damaged heart muscle.
After an MI, if part of the heart muscle has died, it is replaced by scar tissue over the next few weeks.
Who is at risk of having a myocardial infarction / heart attack?
MI is common in people aged over 50 and it becomes more common with increasing age. Sometimes younger people are affected.MI is three times more common in young men than in young women. However, after the menopause, the female hormones no longer protect the heart so the risk is then the same for men and women. Certain risk factors increase the risk of more atheroma forming. The risk factors are :
- Smoking.
- High blood pressure.
- Obesity
- A high cholesterol<.
- Inactivity.
- Diet.
- Diabetes
- Family history
<.
What are the symptoms of a myocardial infarction?
The most common symptom is severe chest pain, which often feels like a heavy pressure feeling on the chest. Pain may travel up the jaw and down the left arm or down both arms. There may be shortness of breath, sweating , feeling sick or faint. The pain may be similar to angina, but it is usually more severe and lasts longer. (Angina usually goes off after a few minutes. MI pain usually lasts more than 15 minutes – sometimes several hours.)
However, some people have only a mild discomfort in their chest or feel like having indigestion or heartburn. Occasionally, an MI happens without causing any pain. Some people collapse and die suddenly. This is not very common.
What should I do if I think I am having a myocardial infarction?
Call for an ambulance immediately. Then, if you have some, take one aspirin tablet.
How is a myocardial infarction diagnosed and assessed?
Myocardial infarction diagnosed and assessed by :
- The symptoms of myocardial infarction.
- An electrocardiogram (ECG). There are typical changes to the normal pattern of the heart tracing in MI.
- Blood tests. A blood test that measures a chemical called troponin and creatine kinase. Damage to heart muscle cells releases these chemicals into the bloodstream.
- Other tests may be done in some cases for example an echocardiogram to diagnose complications such as heart failure.
Also, before discharge from hospital, you may be advised to have tests to assess the severity of atheroma in the coronary arteries. For example exercise tolerance test or an angiography of the coronary arteries may also be performed.
What is the treatment for a myocardial infarction?
There are two treatments that can restore blood flow back through the blocked artery:
- Emergency angioplasty. Ideally this is the best treatment if it is available and can be done within a few hours of symptoms starting. See separate article called Angioplasty for details.
- An injection of a clot-busting medicine is an alternative to emergency angioplasty. It can be given easily and quickly in most situations. Some ambulance crews are trained to give this.
Both the above treatments usually work well to restore blood flow and greatly improve the outlook. The most crucial factor is the speed that one or other treatment is given after symptoms started. Other supportive therapy includes pain relief and oxygen.
Briefly, the following four medicines are commonly prescribed to help prevent a further MI, and to help prevent complications:
- Aspirin – to reduce the stickiness of platelets in the blood, which helps to prevent blood clots forming. If you are not able to take aspirin then an alternative antiplatelet medicine such as clopidogrel or ticagrelor may be advised.
- A beta-blocker medicine – to slow the heart rate and to reduce the chance of abnormal heart rhythms developing.
- An angiotensin-converting enzyme (ACE) inhibitor medicine. ACE inhibitor medicines have a number of actions, including having a protective effect on the heart.
- A statin medicine to lower the cholesterol level in your blood. This helps to prevent the build-up of atheroma.
- Other medicines or treatments may be needed if you develop complications.
Many people recover well from an MI and have no complications. However complications may occur. Some possible complications include the following:
- Heart failure.
- Abnormal heart rhythms
- Collapse and sudden death.
- A further MI may occur sometime in the future.
The most crucial time after a heart attack is during the first day or so. If no complications arise, and you are well after a couple weeks, then you have a good chance of making a full recovery. A main objective then is to get back into normal life, and to minimise the risk of a further MI.
Before discharge from hospital, it is common for a doctor or nurse to advise you how to reduce any risk factors (see above). This advice aims to reduce your risk of a future MI as much as possible.
Reference
Before discharge from hospital, it is common for a doctor or nurse to advise you how to reduce any risk factors (see above). This advice aims to reduce your risk of a future MI as much as possible.
| Last Reviewed | : | 14 November 2014 |
| Writer/Translator | : | Dr. Ainol Shareha bt. Sahar |
| Accreditor | : | Dato’ Dr. Abdul Hadi b. Jaafar |