
Introduction
Burning Mouth Syndrome (BMS) is a chronic oro-facial pain syndrome that affects many adults. It is characterized by burning and painful sensations in the oral cavity with clinically normal mucosa with no known organic cause.
In addition to oral burning , studies shown significant alteration in taste (bitter or metallic), loss of taste, dry mouth, thirst, irritability, depression and decreased desire to socialize.
Synonyms
Glossodynia, Glossopyrosis, Stomatodynia, Stomatopyrosis, Sore tongue and oral Dysesthesia.
Prevalence
Burning mouth syndrome mainly affects women particularly after the menopause, where its prevalence may be 18–33%1.
One study found a prevalence of 4% for the symptom of burning mouth without clinical abnormality of the oral mucosa with the highest prevalence (12%) in women aged 60–69 years1.
Types Of BMS
BMS can divided into 2 categories:
- Primary BMS
- Secondary BMS
Primary BMS is characterized by spontaneous burning pain arising from a visibly intact oral mucosa, normal findings in clinical examination, and no identifiable medical or local dental cause.
Secondary BMS is associated with many local and systemic conditions.
Common causes of BMS
- Local:
- Denture acrylic allergies
- Ill-fitting dentures – mechanical irritation.
- Parafunctional habits – tongue trusting, grinding, clenching, lip sucking and mouth breathing.
- Salivary gland dysfunction – decrease saliva production.
- Taste dysfunction
- Candidiasis
- Viral infections
- Geographic tongue
- Periodontal diseases
- Peripheral nerve damage
- Systemic factors
- Nutritional disorders – iron, B12 and folic acid
- Anaemias
- Central nervous system disorders
- Psychiatric and psychological disorders
- Diabetes Mellitus – predispose to dry mouth and candidiasis
- Sjogren’s syndrome
- Others
- Menopause
- Food and drug allergies
- Medications
 |
 |
|
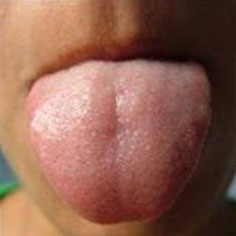
| A normal tongue mucosa is seen in BMS patient | No abnormality of oral mucosa is detected in BMS patients |
Pathogenesis
The aetiology and pathogenesis of burning mouth syndrome is unknown. The aetiology is multi-factorial. Axonal degeneration of glossal terminal nerve fibers, dysfunction of the small diameter afferent sensory fibers, changes in central nervous system and abnormalities in trigeminal somatosensory are shown to be present in BMS patient. These bring to changes in perception of heat, cold, taste and nociceptive stimuli.
Other suggestion on the aetiology is that chronic anxiety or stress results in dysregulation of adrenal steroids which lead to an altered production of neuroactive steroids in skin, mucosa and nervous system.
Another suggested condition is the dramatic fall in gonadal steroids in menopausal patients, will reduce the production of neuroactive steroids thus resulting in neurodegenerative changes in small nerve fibers and areas of the brain related to somatic sensation.
Clinical Features
BMS can be categorized as mild, moderate or severe depending upon intensity of pain. The onset is usually spontaneous and begins late in the morning. The intensity is varied from severe to slight, often at multiple sites, reaching maximum intensity by evening and alters sleeping patterns.
It is more common in women than men (33:1) and most often seen in perimenopausal or postmenopausal women.
Site
The patient complains of burning pain involving the oral mucosa, most common the tongue and/or lips. Other parts that may be affected are hard palate, lip, alveolar ridges, buccal mucosa, oropharynx and floor of the mouth.
Sign And Symptoms
Altered taste disturbances, numbness, tingling and itching can be present.
There may be associated dry mouth (xerostomia).
Treatment
In cases where the etiology is not known, therapy for BMS is symptomatic.
If a systemic condition is responsible for BMS, then appropriate referrals need to be made.
Management protocol for BMS
- Laboratory tests to rule out systemic diseases
- Measurement of parotid stimulated flow rates
- Culture for candida
- Denture evaluation
- Assessment of parafunctional habits
- Psychological assessment of the patient
- Reassurance about cancerophobia
- Pharmacological therapy.
Medication
Antidepressants and benzodiazepines are the mainstay in varied pharmacological therapies employed in treating BMS.
- Alpha-lipoic acid (600mg/day for 20 days, followed by 200mg/day for 10days) – Systemic reviews showed significant improved symptoms compared to placebo.
- Antidepressants – Tricyclic antidepressants like amitriptyline, desipramine, nortriptyline, imipramine and clomipramine appear to be effective in lower doses of 25mg.
- Anxiolytics – the elevated anxiety in patients with BMS may be managed with anxiolytics like chlordiazepoxide, clonazepam and diazepam. Anxiolytics should be used with caution as it could results in dependence. A dose of 15-30mg daily has reported reduction in symptoms.
Conclusion
Burning Mouth Syndrome is a multifactorial disorder with a physiological and psychological basis. Patient reassurance is important.
References
- Burning mouth syndrome: A comprehensive review of literature. Shivpuri A, Sharma S, Trehan M, Gupta N, Asian Journal of Oral and Maxillofacial Surgery 2011; 23: 161-166
- Burning Mouth Syndrome and mast cell activation disorder. BA Lawrence , Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2011; 111: 465-472.
- Psychiatric disorders in burning mouth syndrome. deSouza F, Teixeira AL, Amaral T, dos Santos T et al. Journal of Psychosomatic Research, 2012; 72: 142-146.
| Last Reviewed | : | 20 March 2015 |
| Writer | : | Dr. Hartinie bt. Muhamad |
| Accreditor | : | Dr. Ajura bt. Abdul Jalil |







