Cornea is a transparent dome, which covers the outermost layer of the eye. Its function is to refract light into the retina. Cornea ulcer or infective keratitis is an inflammation of the cornea secondary to infection. It is a serious eye disease because it can lead to permanent vision loss. The cornea can be infected once there is presence of a small corneal wound or injury. The infection can spread deeper into the cornea, which may cause blindness or loss of the eyeball. In 1996, National eye survey reported that cornea ulcer was the fourth cause of blindness in Malaysia1.
Type
Infective corneal ulcer can be divided into four types, based on the type of organism. It is divided into bacterial keratitis, fungal keratitis, viral keratitis and protozoal keratitis. Bacterial keratitis is commonly due to Pseudomonas Aeruginosa, Staphylococcus species and Streptococcus species. Fungal infection is mostly due to Fusarium species, Aspergillous species and Candida species. Viral infection of the cornea is commonly due to Herpes Simplex. Acanthamoeba species is the most common type of protozoa causing keratitis.
Risk factors
The commonest risk factor for corneal ulcer is improper usage of contact lenses. Infection can even in the presence of a minor corneal wound during handling of the contact lens either on insertion or removal. The most common organism causing contact lens related keratitis is Pseudomonas aeruginosa. Fungal infection happens mainly in relation to corneal injury due to trauma and vegetative foreign bodies from agriculture work especially palm oil estate. Other risk factors are chronic ocular surface disease for example, severe dry eye syndrome, exposure keratopathy, neurotrophic keratopathy and uncontrolled usage of topical steroids.
Symptoms and Signs
Patients will present with severe eye pain, foreign body sensation, red eye, tearing, photophobia and blurring of vision. The signs depend on the severity of the ulcer when the patient comes for treatment. Generally, the signs are conjunctival redness and white coloured lesions on the cornea. Severe ulcer will show the presence of pus in the anterior chamber (hypopyon). Advanced ulcer can cause corneal perforation.
 |
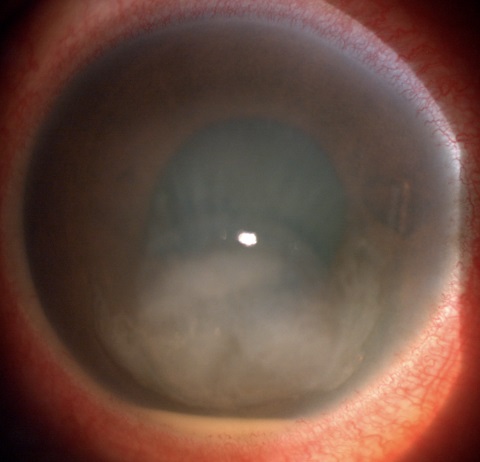 |
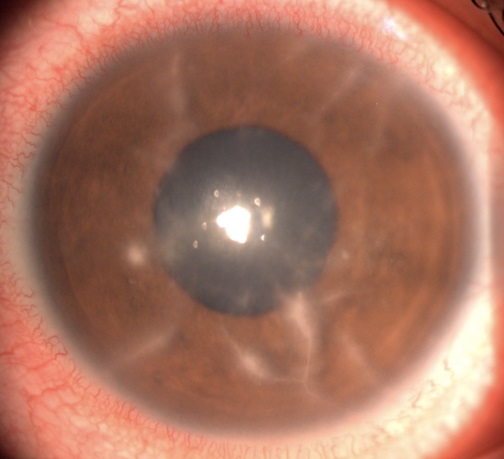
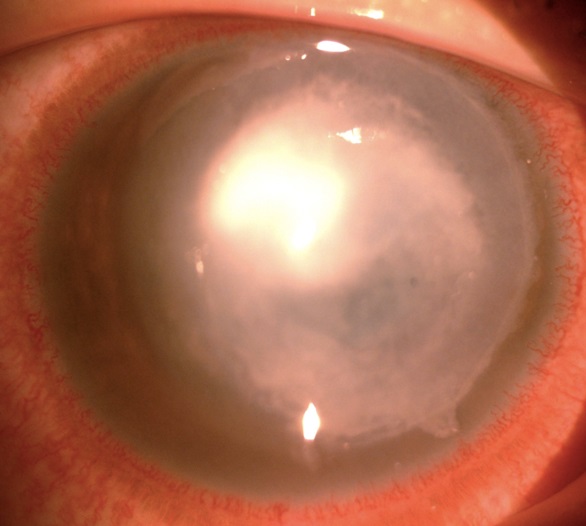
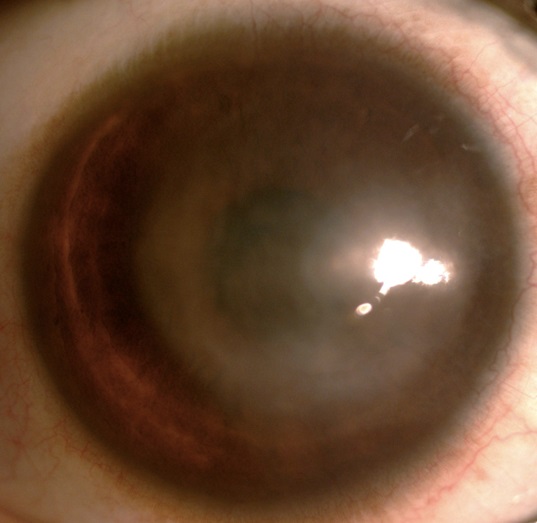
| Acanthamoeba keratitis | Bacterial keratitis |
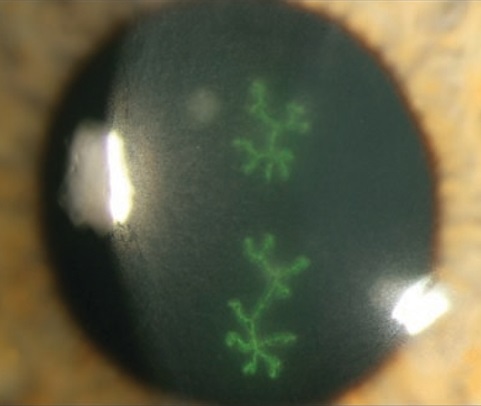 |
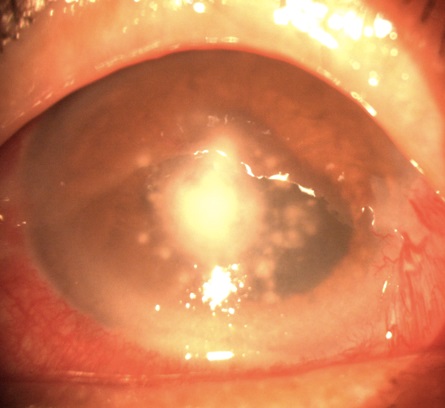 |
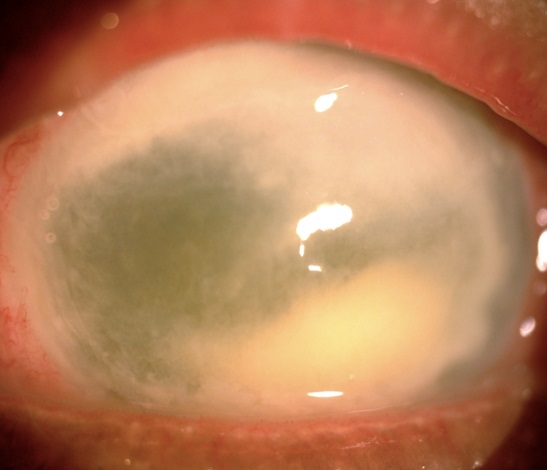
| Viral keratitis | Fungal keratitis |
Investigation
Investigations for corneal ulcer include conjunctival swab, taking samples of infected corneal tissue by corneal scraping, sample of contact lens, contact lens solution and solution from the contact lens case. All these samples are sent to laboratory for gram stain, culture and sensitivity.
Treatment
Patients with corneal ulcer will be treated according to the severity at the time of presentation. The mainstay of treatment is topical eye drops. Systemic medication either oral tablets or intravenous injection, subconjunctival injection and occasionally intrastromal corneal injection may occasionally be used. Types of medication include antibiotic, antifungus, antiviral and antiprotozoa. Treatment will be started immediately and most of the cases require admission to the ward for intensive treatment. Successful medically treated ulcers will form a whitish corneal scar. The corneal scar is permanent and vision will remain poor if the ulcer involves the central visual axis.
The complications of corneal ulcer are corneal perforation and infection involving the whole eye ball (Endophthalmitis) or orbital tissue (Panophthalmitis). A small corneal perforation is managed by cornea gluing but large perforations require corneal transplant. Advanced corneal ulcer, which involves the eyeball and orbit, may require removal of the whole eye tissue (Evisceration).
 |
 |
| Cornea ulcer before and after treatment. The right photo shows corneal scar. |
 |
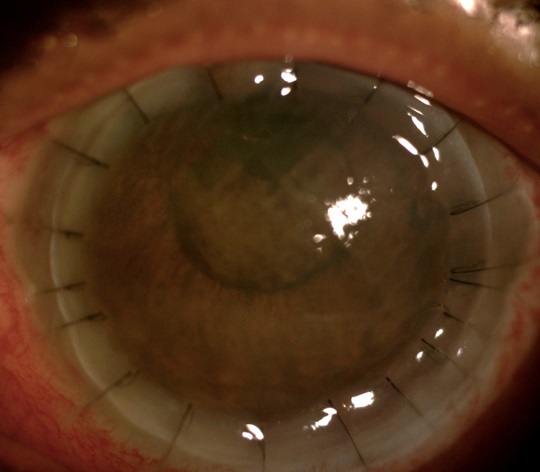 |
| Advanced cornea ulcer before and after cornea transplantation. |
Conclusion
Cornea ulcer is a serious corneal disease which may potentially cause permanent loss of vision. It is important to seek medical treatment from an eye specialist in the presence of eye pain and redness. Early treatment can prevent complications.
Reference
- Zainal M, Ismail SM, Ropilah AR. et al. Prevalence of blindness and low vision in Malaysia population: results from National Eye Survey. Br J Ophthalmol, 1996; 86: 951-956.
- Goh PP, Shamala R, Chandamalar S, Tai XY;National Eye Database Study Group. Contactlens-related corneal ulcer: a two-year review. Med J Malaysia 2010;65:120-123.
- Krachmer, Jay H. Mannis, Mark J. Holland, Edward J.Book Title: Cornea Fundamentals, Diagnosis and Management. 3rd Edition 2011
| Last Reviewed | : | 23 August 2019 |
| Writer | : | Dr. Rohanah bt. Alias |
| Accreditor | : | Dr. Shamala a/p Retnasabapathy |
| Reviewer | : | Dr. Rosniza bt. Ab. Razak |







