Monitoring of Complications
Introduction
ECG is a test assessing the electrical activity of the heart. It is detected by electrodes attached to the outer surface of the skin and recorded by a device external to the body [1]. The electrodes are placed across the chest and it records electrical activity of the heart over a period of time.
ECG measures the rate and regularity of the heart beats. It can also show the size and position of the heart chambers and presence of any damage to the heart.
Most ECGs are performed for diagnostic purposes. It is also recommended for cardiovascular screening in diabetes patients.
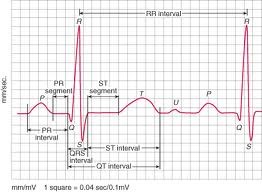
Diagram 1 : Normal electrical activity [2]
Why Must ECG Be Done?
One third of acute myocardial infarction patients have diabetes mellitus and the prevalence is steadily increasing [3]. Early diagnosis of cardiovascular disease is crucial.
ECG detects changes of the heart even before the patients complain of symptoms.
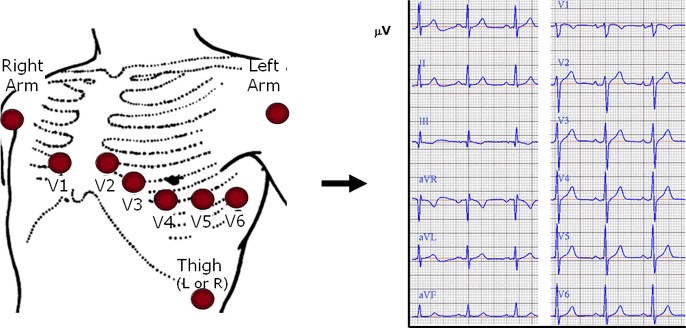
Diagram 2 : Placement of electrodes on the chest and normal ECG recording [2]
What Does It Evaluate?
ECG detects early changes in the heart, for example :
- Ischaemia of the heart muscles
- Delay in the electrical activity of the muscle (prolonged QTc)
- Ventricular hypertrophy (increased thickness of the heart muscles)
ECG may detect ischaemia of the myocardium (heart muscles). Ischaemia is a condition when the heart muscles are deficient of blood supply and oxygen. Fibrotic (scarred tissue muscles consequence to ischeamia) changes at the basal (lower part) area of the left ventricle have frequently been observed in diabetes patients. This cardiac involvement can be detected even before clinical evidence is apparent.
A study (EURODIAB) on diabetes individuals with normal QTc (electrical activity – refer to the diagram below) at baseline was examined [4]. Prolonged QTc (delayed in electrical current of the heart muscle) was associated with female sex, uncontrolled blood sugar and high systolic blood pressure [4]. Physical activity and normal body mass index were protective factors [4].
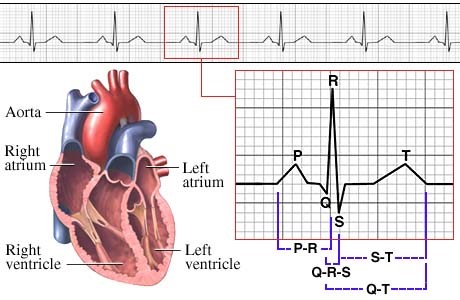
Diagram 3
Prevalence of left ventricular hypertrophy (increased thickness of the left ventricle) was found to be 3 times greater in diabetes patients compared to general population [5]. These diabetes patients may not usually experience any chest discomfort (asymptomatic).
These evidences strongly advocate ECG testing for all diabetes patients at least annually even if asymptomatic [6].
In view of the autonomic neuropathy (nerve function abnormality) in diabetes patients, myocardial ischaemia is often painless [7]. Resting ECG abnormalities and cardiac autonomic dysfunction can be detected by routine screening. Autonomic dysfunction is a condition where there is abnormal nerve activities leading to irregularity of the electrical activities of the heart muscles. They were found to be predictors of silent ischaemia in asymptomatic type 1 diabetes mellitus [8,9].
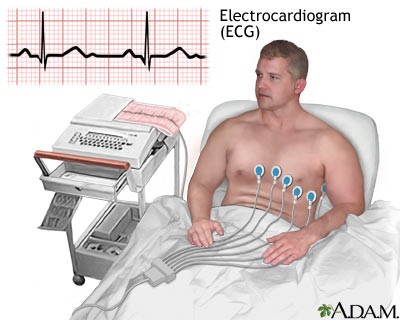
Diagram 4 : How resting ECG is conducted [2]
What To Do If The ECG Is Abnormal?
Abnormal ECG needs further evaluation and assessment by the doctors. Management must be based on clinical findings and history from the patients. Cardiologist assessment is advocated.
How Often Should ECG Be Done?
ECG must be done at least once a year. More frequent ECG testing is necessary if the patient is symptomatic or he/she is a known case of ischaemic heart disease.
Conclusion
ECG is an important test used for screening cardiovascular disease in diabetes patients. It should be done at least annually even if the patient is asymptomatic.
References :
- http://en.wikipedia.org/wiki/Electrocardiography – accessed 21st September 2012.
- http://www.google.com.my/search – accessed 21st September 2012 (pictures).
- Shlomo Stern, Samuel Sclarowsky, The ECG in Diabetes Mellitus. Circulation 2009; 120: 1633 – 1636.
- Giunti S, Bruno G, Lillaz E, Gruden G, Lolli V, Chaturvedi N, Fuller JH, Veglio M, Cavallo-Perrin P. Incidence and risk factors of prolonged QTc interval in type 1 diabetes. The EURODIAB Prospective Complications Study. Diabetes Care. 2007; 30: 2057–2063.
- Giunti S, Bruno G, Veglio M, Gruden G, Webb DJ, Livingstone S, Chaturvedi N, Fuller JH, Perin PC. Electrocardiographic left ventricular hypertrophy in type 1 diabetes. Diabetes Care. 2005; 28: 2255–2257.
- Malaysian Clinical Practice Guideline on Management of Type 2 Diabetes Mellitus 2009.
- Raman M, Nesto RW. Heart disease in diabetes mellitus. Endocrinol Metab Clin North Am. 1996; 25: 425–438.
- Dweck M, Campbell IW, Miller D, Francis CM. Clinical aspects of silent myocardial ischemia: with particular reference to diabetes mellitus. Br J Diabetes Vasc Dis. 2009; 9: 110–116.
- Wackers FJTh, Young LH, Inzucchi SE, Chyun DA, Davey JA, Barrett EJ, Taillefer R, Wittlin SD, Heller GV, Filipchuk N, Engel S, Ratner RE, Iskandrian AE. Detection of silent myocardial ischemia in asymptomatic diabetic subjects. Diabetes Care. 2004; 27: 1954–1961.
| Last reviewed | : | 13 January 2014 |
| Writer | : | Dr. Sri Wahyu binti Taher |







