Gallstone disease is a common medical condition in Malaysia. This is associated with the increasing consumption of fatty food. With advances in radiological services, more patients are diagnosed with Gallstones. It is unique disease as it involves 3 organs namely the liver, gallbladder and pancreas. The clinical presentation varies depending on whether the bile flow is obstructed. Laparoscopic surgery offers a faster recovery and return to daily activities.
What is gallbladder and its function
The gallbladder is an organ located under the liver It functions as a store for bile produced by the liver. Bile is essential for the absorption and digestion of fat. When the semi-digested food passes the upper part of the small intestine called duodenum, a hormone called Cholecystokinin is released which stimulates bile release.
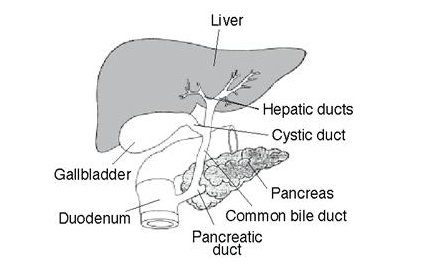
Figure 1: Anatomy of liver, gallbladder and duodenum
Bile contains water, cholesterol, fats, bile salts, proteins, and bilirubin. Bilirubin is considered an end product of red blood cells. Cholesterol, bile salts and bilirubin are the three main components that determine the formation of gallstones.
What is Gallstone
Gallstones are stone like formations that develop in the gallbladder and found in many shapes, colour and consistency. It is formed when one of the three main components in the bile (cholesterol, bile salts and bilirubin) is in excess causing imbalance in its liquidity. Over time these stones enlarge in size or number. Gallstones may get trapped along the cystic or common bile duct as they expelled from the gallbladder. Stones may also occur primarily in the liver, hepatic ducts or the common bile duct. Stones are classified according to their chemical components into cholesterol stones, pigment stones and mixed stones. The majority are mixed stones.

Figure 2: Typical cholesterol stones retrieved from gallbladder
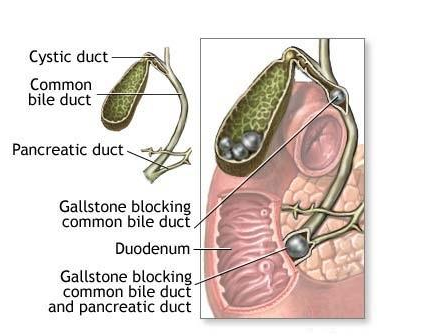
Figure 3: An illustration showing two different sites of bile stone formation; in the gallbladder and the common bile duct
There are several factors that may influence the formation of bile stone or gallstones. They are :
- Sex. Women are at higher risk, twice as likely as men. This is caused by the higher amount of hormone oestrogen found in women. Certain conditions among women expose them to an even higher amount of oestrogen such as pregnancy, hormone replacement therapy and birth control pills. Excess oestrogen increases cholesterol level in bile thus disrupting the equilibrium in bile liquidity. Excess oestrogen also decreases gallbladder contractility leading to bile stasis and gallstones formation.
- Weight. Obesity is another risk factor due to higher cholesterol levels in the blood.
- Diet. Diet high in fats and cholesterol.
- Age. Elderly individuals above the age of 60 have higher incidence of Gallstones.
- Diabetes. Individuals with diabetes mellitus carry higher amount of fatty acids namely triglyceride and cholesterol in their blood circulation.
- Cholesterol-lowering drugs. Drugs that lower cholesterol levels in the blood also increase the amount of cholesterol secreted into bile.
Haemolytic anaemia. A condition where the red blood cells are destroyed due to an underlying problem. Heme, a by-product of red blood cells destruction is metabolized into bilirubin.
What are the symptoms of bile stones or gallstone disease
Majority of gallstones (bile stones in the gallbladder) do not cause any symptoms. It may be found as an incidental finding during a routine investigation. A small percentage of gallstones may cause symptoms such as pain called gallstone colic at the right upper quadrant of the abdomen, lasting for several minutes. Gallstone colic is commonly accompanied by nausea and vomiting. It is usually self-remitting but it may recur intermittently. Inflammation of the gallbladder or infection of the static bile is termed acute cholecystitis and it may produce fever.
If the stone blocks the central passage of bile flow from the liver to duodenum, it will cause congestion of the liver with excess bile. This excess bile will spill over into the systemic circulation causing jaundice or yellowish discolouration of the eye, skin and mucous membrane. In severe cases excess bilirubin deposition in the skin causes itchiness. The other common symptoms are described above such as colicky pain, nausea and vomiting. Infection of the static bile presents with fever and is termed Ascending Cholangitis. If left untreated it may be fatal.
A stone at the distal end of the common bile duct will also obstruct the flow of pancreatic enzymes from the pancreas as common bile duct and pancreatic duct share a common outflow passage into the duodenum called the Ampulla of Vater. Blockage to the flow of pancreatic enzymes will eventually cause inflammation of the pancreas, a condition called Acute Pancreatitis. It causes severe pain at the central upper part of the abdomen that may radiate to the back.
How to diagnose bile stones or gallstones disease
If an individual presents with symptoms mentioned above, the usual method confirming the disease are as follows
- Blood tests. These are essential investigations to determine the status of illness. Specific blood investigations such as the while cell counts, liver function tests and serum amylase are particularly important to confirm infection, obstruction and pancreatitis.
- Abdominal X-Ray. Ten percent of bile stones are radio-opaque, meaning that they can be seen on plain x-ray. They are usually incidental findings on tests done for other purposes. X-Rays are not important diagnostic tools for this disease.
- Ultrasound. This is a simple and fast non-invasive imaging technique that is commonly used to diagnose gallstone disease. It can also determine if there is obstruction to the flow of bile. However small stones may pose difficulty in diagnosis especially if the ducts are obscured by the air in the bowel.
- Computerized tomography scan or CT scan. This is also a non-invasive imaging technique that uses x-ray to produce cross-section images of the body. CT scan will definitely help to determine inconclusive ultrasound results especially in evaluating distal common bile duct obstruction.
- Endoscopic retrograde cholangio-pancreatography or ERCP. This is an endoscopic procedure with additional use of fluoroscopy or contrast media injected through the bile ducts and images are visualized by X-Ray. Its role as a diagnostic tool has lessened with the availability of non-invasive imaging technique. The current usa of ERCP is mainly therapeutic to remove stones in the bile ducts.

Figure 4: A surgeon performing therapeutic ERCP to remove bile duct stones. Patient is sedated throughout the procedure
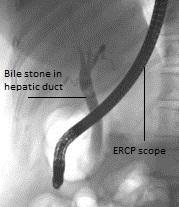
Figure 5: An ERCP image showing bile stones in the hepatic duct
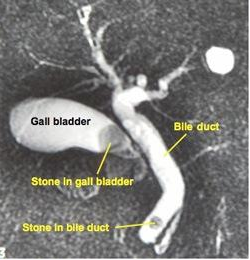
Figure 6: An imaging showing two different sites of bile stone formation; in the gallbladder and the distal common bile duct
Treatment of bile stones or gallstone disease
Treatment for bile stones or gallstone disease depends on the symptoms and its location. The majority of asymptomatic gallstones do not require treatment. However surgery may be necessary in certain situations. Discussion with a surgeon would be advised in such circumstances.
Symptomatic gallstones are treated by admission to ward and treatment with pain killer, anti-spasmodic medication and antibiotics if there are signs of infection. Upon symptom resolution, patients are offered to remove the gallbladder, a procedure called cholecystectomy, which is done on a planned admission. This surgery is done mainly through a laparoscopic approach or key-hole surgery. Camera and surgical instruments are inserted into the abdominal cavity through 3 or 4 small 0.5 cm – 1.0 cm incision on the abdomen. Laparoscopic surgery causes less post-operative pain with faster recovery and return to normal activities. Occasionally cholecystectomy is performed via a conventional open method especially during emergency or when the surgeon encounters difficulties during laparoscopic surgery.

Figure 7: The small nature of the wounds involved in laparoscopic cholecystectomy offers fast post-operative recovery and return to daily activities. Small 0.5 cm – 1.0 cm incision marked x
If acute cholecsytitis does not resolve with antibiotics, emergency cholecystectomy is performed, which is commonly done via open method.

Figure 8: The conventional or open cholecystectomy performed through 10 – 15 cm incision at the right upper quadrant of the abdomen

Figure 9: A complete specimen of the gallbladder after cholecystectomy

Figure 10: A close-up view of a cut-open specimen of the gallbladder revealing a cholesterol stone and bile sludge
When a patient presents with jaundice associated with biliary obstruction, they are treated in a similar manner as symptomatic gallstones.However soon after the infection and colic has resolved, they will undergo ERCP to remove the biliary stones. It is usually this is done during the same admission. ERCP may also be done as an emergency procedure if the patient does not show any improvement with antibiotic or too ill for surgery. In this situation a plastic stent is inserted to relieve the obstruction and ensure that the bile flow into the duodenum. Cholecystectomy can be performed once the patient improves.
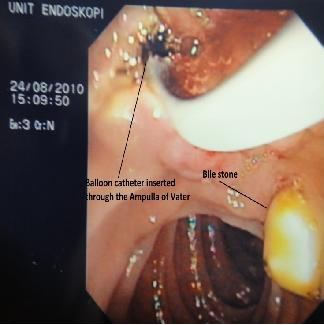
Figure 11: Multiple cholesterol stones with bile sludge after being removed from the gallbladder through ERCP
Occasionally the obstructed biliary stone is removed during open Cholecystectomy. However this involves surgically opening up the bile duct. Hence to ensure that the bile duct heals without surgical stricture or stenosis, a rubber T-shape tube is placed into the common bile duct. This tube will be removed after 6 weeks.

Figure 12: Biliary drainage with T-tube after surgical exploration of the bile duct and removal of biliary stone
Non-surgical approach or medication may also be used to treat gallstone disease. The usage of such medication or oral dissolution therapy have limited role due to its low effectiveness and high recurrence rate. It is only used in situations where the patient has a high surgical or anaesthetic risk.
| Last Reviewed | : | 20 June 2014 |
| Writer | : | Dr. Mohamad Shukri Jahit |
| Accreditor | : | Mr. Fitjerald Henry |
| Reviewer | : | Dr. Hamiza bt. Shahar |







