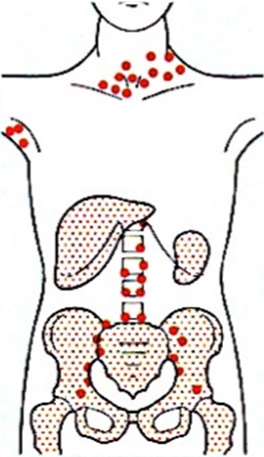
Lymphoma is a cancer that stars in cells called lymphocytes, which are part of the body’s immune system. Like any other types of cancer, lymphoma are divided to certain subtypes, almost 35 of them had been identified, depending on types of the involved cells.
The lymph system (also known as the lymphatic system) is composed mainly of lymphoid tissue, lymph vessels, and a clear fluid called lymph. The lymph nodes are connected by a system of lymph vessels. These vessels are like veins, except that instead of carrying blood, they carry lymph and lymphocytes. Lymph nodes get bigger when they fight infection. The main types of lymphocytes are B lymphocytes (B cells) and T lymphocytes (T cells). Normal B cells and T cells do different jobs within the immune system.
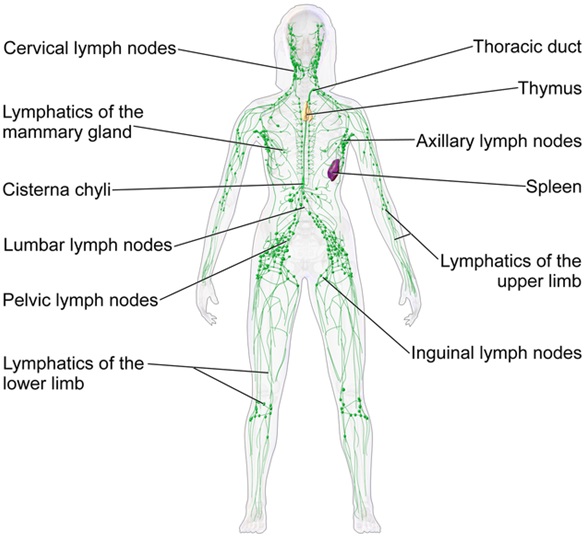 |
| The Lymphatic System |
Cancer starts when cells in the body begin to grow out of control. The big problem is that these cells start to divide before they are fully mature. So they can’t fight infection as normal white blood cells do. The abnormal lymphocytes start to collect in the lymph nodes or in the other places such as the bone narrow or spleen. They can then grow into tumors and begin to cause problems within the lymphatic system or the organ, in which they are growing, for example in the brain tissue, colon, bones, lungs and the bone marrow. This will lead to main organ dysfunction and health deterioration, and finally death if not being treated early.
There are 2 main types of lymphoma, i.e. Hodgkin Lymphoma and Non Hodgkin Lymphoma (NHL). Both types have similar symptoms and lymph nodes enlargement can happen anywhere in the body. To get a correct diagnosis is important, as it carries different treatment and prognosis. Diagnosis can be obtained by specific tests available for each typed of lymphoma, and the process can be time consuming, as some types are difficult to be diagnosed, which needs expert review in the histopathology, molecular and genetic testing.
Causes
We don’t know the cause in most people who get lymphoma. But there are some factors that increase the risk.
- Age : Incidence increased with increasing ag. In youg adult age between 20 to 24 years old, the incidences is 2.4 cases in 100 000, but increased to 46 cases in 100 000 among elderly age 60 to 64 years old.
- Bacterial and virus infection, such as HIV, EBV, helicobacter pylori, hepatitis B and C.
- People whose immune system is not working as well as it should are more likely to develop lymphoma. Immunity can be lowered for the following reasons :
- Taking drugs to stop organ rejection after a transplant
- HIV and AIDS
- Being born with rare medical conditions which affects immunity
- Autoimmune disease
- Exposure to toxic agents : pesticide, benzene
- Genetic predisposition or family history of cancer
 |
|
Cervical Lymph Node Enlargement |
Symptoms
- Swollen, painless lymph nodes in the neck, armpits, or groin.
- Fever
- Loss of appetite
- Unexplained weight loss
- Weakness and tiredness that don’t go away (fatigue)
- Itching of the skin
- Other symptoms related to lymph modes enlargement in the specific organs such as cough and shortness of breath (lungs), bloody stool (colon), headache and seizure (brain) or paralyze (nervous system)
If patients have been complaining of any of the above symptoms, a complete physical examination will be performed by doctor, followed by few lac tests as listed:
- Blood tests: A complete Blood Count (CBC) will usually be performed to check the number of white blood cells. Additional tests might include a lactate dehydrogenase level (can be elevated in lymphoma).
- Lymph node biopsy : The swollen lymph node is removed, either part or all of it, and look at it under a microscope. If the enlarged node is near the surface of the skin, the whole lymph node will be removed. This is called an excision biopsy. It is done under local or general anaesthetic, usually as a day care. If the enlarged lymph node is deeper in the body, a needle is used to take a sample of tissue with help of an ultrasound scan or CT scan. This is called an ultrasound or CT guided core biopsy. It is usually done under local anaesthetic in the radiology department.
- Imaging procedures: A chest X-ray or CT scan of the chest or neck might help detect the presence of tumours or more enlarged lymph nodes determine the lymphoma stage. Positron Emission Tomography (PET) scanning is a newer modality to help detect lymphoma.
- Bone marrow biopsy: A bone marrow biopsy can establish the spread of the disease. This involves the insertion of a needle into the bone to obtain bone marrow. In adults, the most common site for this biopsy is the pelvic bone, and it is done under local anaesthesia or sedation.
 |
|
Excision Biopsy of Lymph Node |
Treatment
Treatment of lymphoma is tailored to disease type, disease stage, and an assessment of the risk of resistant disease. Before starting treatment, a counseling will be done by doctor on treatment schedule, all related side effects and disease prognosis. His is important as treatment will take about 6 to 8 months, and full support from patient and family members are needed fir a successful treatment.
Stage of Lymphoma
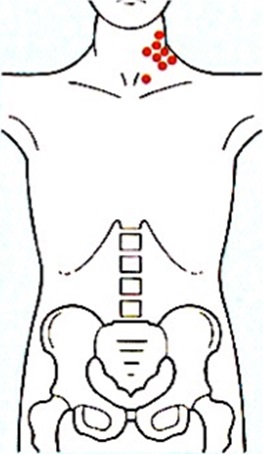 |
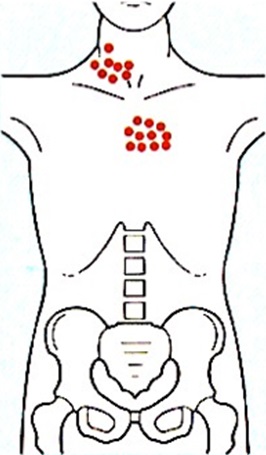 |
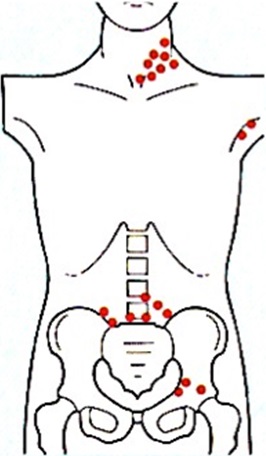 |
 |
| Stage 1: Involvement of single lymph node region or single extralymphatic site (lE) |
Stage 2: Involvement of two or more lymph node regions on same side of diaphragm; may include localized extralymphatic |
Stage 3: Involvement of lymph node regions on both sides of the diaphragm; may include spleen (llls) or localized |
Stage 4: Diffuse extralymphatic disease (e.g. in liver, bone marrow, lung, skin) |
Generally, treatment are divided into different types according to the type and stage of lymphoma, as follows:
- Surgery
- Only for early or limited stage 1 Hodgkin’s lymphoma, involving non lymphoid organ i.e. stomach, thyroid or splenic lymphoma.
- Radiation therapy
- Radiation therapy uses high-energy rays (or particles) to destroy cancer cells.
- Can be used in lymphoma stage 1 or 2, but if advanced stage, it is combined with systematic chemotherapy.
- People who are getting a stem cell transplant mat get radiation to the whole body along with high-dose chemotherapy, to try to kill lymphoma cells throughout the body.
- Also as a form of palliative care advanced stage disease, i.e. spinal and brain irradiation.
- Chemotherapy and chemo immunotherapy
- This is a drug treatment either as an injection or oral form that kills cancer cells. But other cells in the body, such as those in the bone marrow, the lining of the mouth and intestines, and the hair follicles, also divide quickly. These cells are also likely to be affected by chemotherapy, which can lead to certain side effects.
- The side effects can include hair loss, mouth sores, loss of appetite, nausea and vomiting, diarrhea, low blood cell counts (hemoglobin, platelets, and white cells count). Organ toxicity of main organs also can happen i.e. heart, lungs and kidneys after repeated course of chemotherapy treatment.
- Many chemo drugs can affect fertility (the ability to have children) and secondary malignancy that might not occur until 5 to 10 years after treatment.
- Immunotherapy is treatment that either boost the patient’s own immune system or uses man-made versions of the normal parts of the immune system. These treatment may kill lymphoma cells or slow their growth. It is often used in combination with chemotherapy.
- The chemotherapy drugs can be delivered orally or intravenously, but it will not reach the fluid around the spinal cord. Prophylaxis Intrathecal Chemotherapy is the injection of chemo drugs into the fluid around the spinal cord to prevent cancer spread to the brain in certain types of lymphoma.
- Bone marrow or stem cell transplant
- The treatment involved very high doses of chemotherapy such as the BEAM combination, sometimes with radiotherapy. It aims to try to cure some types of cancer. High dose treatment with a stem cell transplant can give a better chance of curing some types of NHL, or controlling it for a longer time, than standard chemotherapy.
- The stem cell collection is done by apheresis machine (as in the figure shown below)
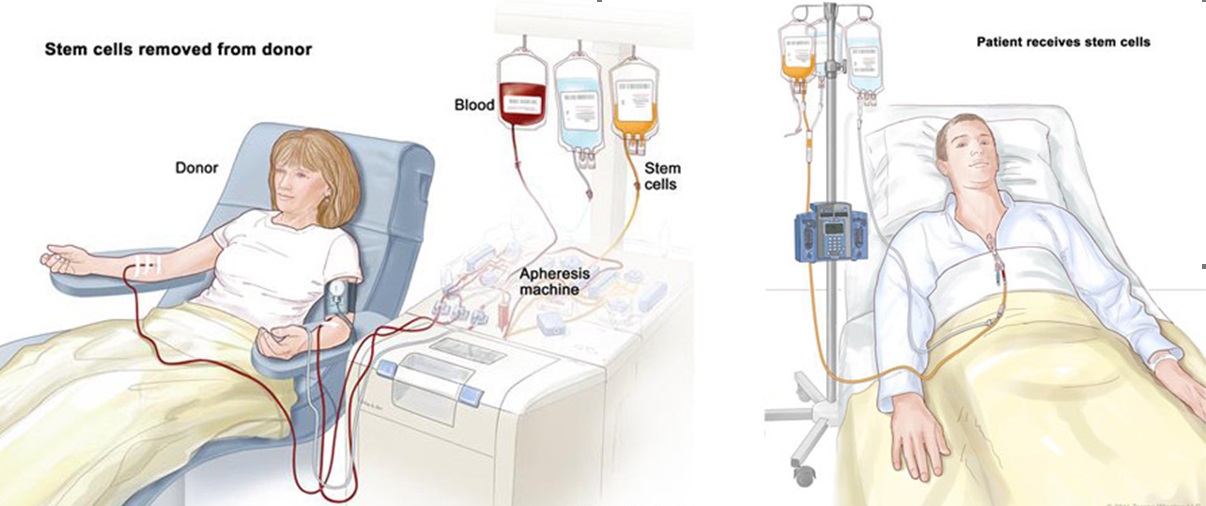 |
| Allogenic Stem Cell Transplant |
Prognosis
The prognosis of lymphoma can be good but is linked to the type of disease, the extent of spread (staging), and response to therapy. Prognosis should be discussed with the patient’s health-care provider.
Five year survival is a measure used to predict and gauge the severity of the cancer. Patient’s should discuss risk factors, staging, and classification with their health-care team as none of these numbers should be applied to an individual patient without considering all the circumstances of the patient’s illness.
Generally, the 5 – year survival rate for patient with non-Hodgkin’s lymphoma is 69%. For Hodgkin’s lymphoma, the 5-year survival rate is better, i.e. 91-94% for stage 1 and 2, 59-90% for stage 3 and 4. Hence, lifelong monitoring is important, even if the patient has completed treatment. Some of lymphomas may relapse, even after treatment finished, and the patient will need salvage chemotherapy and stem cell transplant.
Reference
- Hodgkin Lymphoma Treatment & Management, Bradley W Lash, MD, Nov 6, 2014, Medscape.
- Non-Hodgkin lymphoma detailed guide ,American Cancer Society.Cancer, Facts & Figures 2015 Atlanta.
- Non-Hodgkin’s Lymphoma, Medicinenet.com , April 27, 2015.
- Cancer Research UK, updated : 29 December 2014.
| Last Reviewed | : | 29 May 2017 |
| Writer/Translator | : | Dr. Shahada Sobah bt. Abdul Hamid |
| Accreditor | : | Dr. Jameela bt. Sathar |







