Introductions
Mucocele is one of the causes of a swelling in your mouth. It is a common lesion of the oral mucosa characterized by single or multiple, spherical, fluctuant nodules which are generally asymptomatic.
Clinical Features
Mucoceles are most common in children and young adults, a fact probably related to the higher frequency of injuries. According to several studies, the lower lip is the region most affected by mucoceles. However, rare cases of mucoceles involving the upper lip, palate, retromolar region, buccal mucosa, lingual frenum, and dorsal tongue have been reported. The diameter of mucoceles range from a few millimeters to centimeters. Many patients report the periodic discharge of viscous fluid from the lesion.
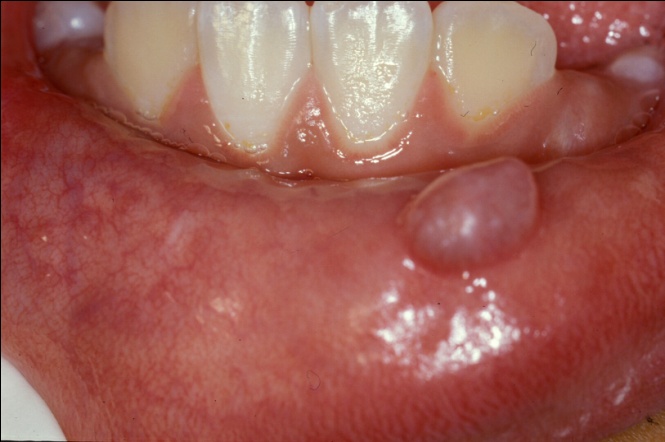
Figure 1: Translucent-blue nodule on the lower labial mucosa.
Picture source : http://oralmaxillo-facialsurgery.blogspot.com
Ranula
Ranula is the designated term for mucoceles located on the floor of the mouth. The name is derived from the Latin word “rana” (meaning frog) because of its resemblance with the underbelly of a frog. Ranulas are generally related to the duct systems of the sublingual salivary glands and, less frequently, to the submandibular gland and minor salivary gland ducts of the floor of the mouth. A ranula manifests as a cup-shaped fluctuant bluish swelling on the floor of the mouth. Ranulas tend to be larger than mucoceles located in other regions of the mouth, reaching some centimeters in diameter. Depending on size and location, patient may present external swelling and relate discomfort, interference with speech, mastication, and swallowing.

Figure 2: A large fluctuant swelling on the floor of the mouth called as ranula.
Picture source : https://www.ebmedicine.net
Pathogenesis
Mucocele are believed to result from mechanical trauma to the excretory duct of the salivary glands, causing duct rupture, with consequent extravasation of mucin to the connective tissue stroma (mucus extravasation phenomenon, MEP) (Fig. 3). In addition, mucus might be retained in the duct and/or acinus as a result of duct obstruction (mucus retention phenomenon, MRP). MRP are less frequent and are seen particularly in the elderly. Mucus extravasation triggers a secondary inflammatory reaction predominantly consisting of inflammatory cells in surrounding connective tissue, followed by a granulation tissue-type reaction that culminates in the formation of a fibrous capsule around the mucin deposit, conferring a cyst-like aspect to the lesion.
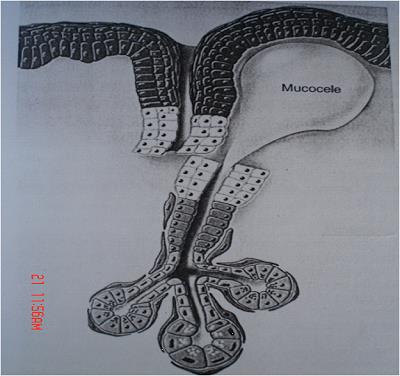
Figure 3: Mechanical trauma to the excretory duct of the salivary glands, causing duct transection or rupture, with consequent extravasation of mucin to the connective tissue stroma.
Picture source : http://dentistryandmedicine.blogspot.com
Histopathological Features
Microscopically, the lesion typically consists of a mucin-filled cystic cavity or cavities lined by inflamed granulation tissue (Fig . 4). There is no epithelial lining. The extravasated mucous evokes a chronic inflammatory reaction and the wall of the cyst is infiltrated by large numbers of macrophages with vacuolated cytoplasm containing phagocytosed mucin (Fig. 5). Similar cells are seen within the cyst lumen. In some cases the mucous is present as diffuse pools rather than being contained within a more or less discrete cyst-like space.
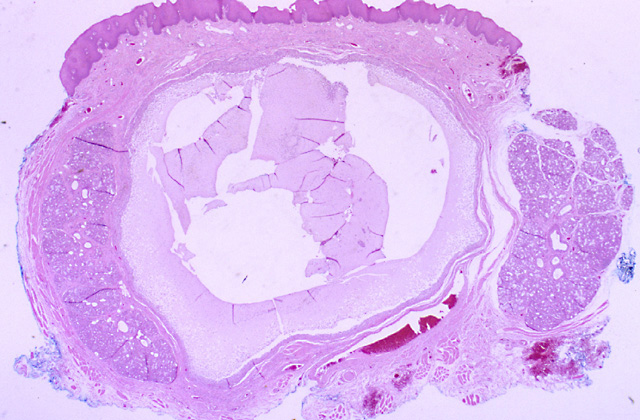
Figure 4: Photomicrograph of a mucocele showing cystic space filled with mucinous exhudates and lined by granulation tissue.
Picture source : http://emedicine.medscape.com
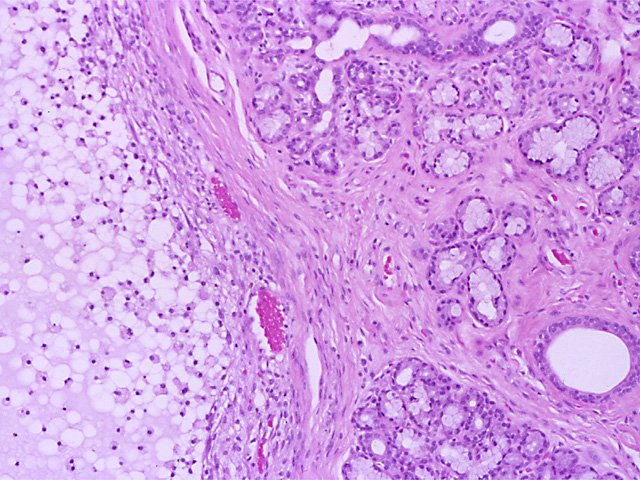
Figure 5: Higher magnification reveals the cyst wall and the lumen are infiltrated by large numbers of foamy macrophages.
Picture source : http://emedicine.medscape.com
Treatment
Mucoceles are more frequently treated by surgical excision of the lesion and careful dissection of the adjacent minor salivary glands affected (Figure 6). However, recurrence can occur and a new surgical intervention taking the above mentioned care is necessary. In the case of ranulas, treatment consists of surgical removal of the sublingual gland and/or marsupialization (Figure 7). Marsupialization may be performed before definitive excision of the gland in an attempt to permit the formation of an intraoral fistula through which saliva is excreted. This approach requires the removal of the roof of the lesion in order to permit reestablishment of the communication between the gland duct and oral cavity.

Figure 6: Surgical removal of mucocele of lower lip.
Picture source : http://pixgood.com
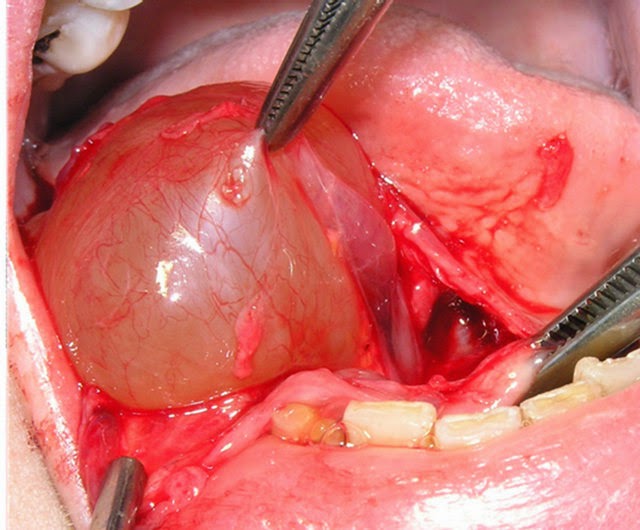
Figure 7: Surgical removal of ranula of the left floor of mouth.
Picture source : http://entsurg.blogspot.com
References
- Chrispian Scully. Oral and Maxillofacial Medicine: The Basis of Diagnosis and Treatment. Elsevier Health Sciences, 2008.
- Joseph A. Regezi, James J. Sciubba, Richard C.K Jordan. Regezi: Oral Pathology: Clinical Pathologic Correlations, 5th ed. Saunders, An Imprint of Elsevier, 2008.
- J.V. Soames and J.C. Southam. Oral Pathology-4th Ed. Oxford University Press, 2005.
| Last Reviewed | : | 11 November 2015 |
| Writer | : | Dr. Khamisah bt. Awang Kechik |
| Accreditor | : | Dr. Hans Prakash a/l Sathasivam |







