Introduction
There are many organization bodies and agencies who involve in the development of standards for radiation protection. These organizations also involve in establishing new regulation for the protection against hazards caused by ionizing radiation used in medical fields. Examples of international organizations involve are International Commission on Radiological Protection (ICRP), National Council on Radiation Protection and Measurements (NCRP), United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR) and National Academy of Sciences Advisory Committee on the Biological Effects of Ionizing Radiation (NAS-BEIR).
In Malaysia, the used of ionizing radiation is controlled by the Atomic Energy Licensing Act 1984 (Act 304) that includes both the use of medical and non-medical applications. The authority for the use of medical application is Director General of Health, Ministry of Health (MOH). There a few regulations under the Act 304 includes Atomic Energy Licensing (Licensing) Regulations 1986, Atomic Energy Licensing (Basic Safety Radiation Protection – BSRP) Regulations 2010 and Atomic Energy Licensing (Radioactive Waste Management) Regulations 2011. The Act 304 and its subsidiary regulations explains the concepts and principles of radiation protection to patients, radiation workers as well as public members in details.
Radiation Protection Principles
The use of radiation in medicine should be justified and optimized as recommended in the BSRP 2010. In addition, ICRP has worked for several decades to develop the radiation protection philosophy based on a broad scientific basis, and formulated some fundamental principles given by the key words justification, optimization and dose limitation. However, the dose limits do not apply to the radiation protection of patients.
Justification of medical exposure is primarily the responsibility of the doctors. In addition, mass screening must be justified by weighting the total benefit against the total detriment of the radiation exposure. It is also applicable to medico-legal or insurance purposes. In addition, benefits to society as a whole can be considered in the justification process.
A basic principle of radiation protection in patients is the need to maintain exposure to ionizing radiation at a level of As Low As Reasonably Achievable (ALARA), with economic and social factors are taken into consideration. Implementation of ALARA principle is achieved by application of the basic principles of radiation protection. The radiologists and radiographers have to educate patients with sufficient information regarding the radiological examinations and to assure the patient that the benefit is outweights the risk. One of the best accepted methods of providing this information is through comparison of relative radiation risks.
| Scaled Relative Dose | |
| Natural background | 50 – 100 chest examinations/year |
| Diagnostic radiology | 0.1 – 500 chest examination/study |
| Nuclear imaging | 50 – 1,000 chest examination/study |
| Start of acute radiation syndrome | 30,000 chest examinations in one day |
| Lethal dose | 30,000 chest examinations in one day |
| Radiation therapy (small volume of tissue) | 100,000 – 1,000,000 chest examinations in a few weeks |
| Ultrasound | This scale does not apply |
| Magnetic Resonance Imaging (MRI) | This scale does not apply |
Table 1: Comparison of Relative Radiation Levels
It is also important to know that patient has the right to refuse radiographic examination, and the radiographer or doctors is bound by professional duty to respect patients right.
Protection of the Patients
The radiographers are responsible to ensure that patients are worn proper protective devices to minimize patient exposure while producing a satisfactory diagnostic image. Personal protective devices includes gonad shielding, lead apron, thyroid shielding and goggle. Some organs are sensitive to the radiation such as kidneys, female breast and the lens of the eye. For example, chest PA examination reduces dose to the breast because the x-ray beam produces from behind our body. In fact, shielding the gonad, ie. the ovaries or testis is important to minimize the possibility of any genetic effect in the future. Gonad shielding is extremely effective in reducing dose to the gonads. In addition, shielding the gonad of children and adults of childbearing ages are also important.
Lead aprons are also used to protect patient from unnecessary x-ray radiation exposure from radiological procedures. Lead apron is designed to shield the body from harmful radiation. It is important to remember that the used of lead apron only effective if it is wear properly, matched with the appropriate radiation energy.
The radiographer has to ensure that the size of the x-ray beam should always be restricted to the area of clinical interest and should never exceed the size of the image receptor. Proper collimation not only reduces patients dose but also improves the overall image quality because less scatter radiation is created with smaller field sizes.
Technique factors are also important to produce good image quality with less dose to the patients. High kVp and low mAs technique are preferred to decrease patient dose. Proper technique factors choosen are the responsibility of radiographer.
In radiographic, the grids are placed between the patient and image receptor to absorb scatter radiation. Grids will absorb primary radiation as well as scatter radiation. The lowest possible of grid ratio consistent with scatter removal should be utilized to keep patient dose as low as reasonably achievable.
Radiation Exposure of the Pregnant Patients
Special consideration is taken into account of radiation exposure during the early weeks of pregnancy, generally before the woman is aware of her condition. The dose to the foetus is much more concern, particularly in the early stages of development when certain tissues and organs are especially sensitive to radiation. Foetus may be particularly radiosensitive during the period of 8 to 15 weeks postconception. Care must be taken to reduce radiation exposure to any women including pregnant or potentially pregnant patients. Currently, BSRP 2010 recommend the dose limit for foetus of not exceed 1 mSv per year.
Figure 1: Signage for pregnant or potentially pregnant patients outside the x-ray room
To minimize the possible exposure to an embryo in the earliest days of pregnancy, a guidance known as the 28-day rules was recommended. In many radiology department, female patient in childbearing ages are asked to provide the date of their last menstrual period (LMP). If the patient concern about the possibility of pregnancy, the examination may be reschedule. If the radiological examination are performed, a medical physicist should perform calculation to estimate the actual fetal dose.
Diagnostic Reference Levels (DRLs)
For medical exposures of patients as part of their investigation or treatment, dose limits have not been specified in the ICRP reports or BSRP 2010, since such exposures are intended to provide a direct benefit to the exposed individual. The diagnostic reference levels (DRLs) is recommended for use as a guide for medical exposure from various examinations and also to avoid unnecessarily high doses to the patient. DRLs are part of the optimization process. It is essential to assure that image quality appropriate for the diagnostic purpose is achieved when changing patient doses. Good image quality must be maintained at the appropriate level as radiation doses are decreased.
The MOH has carried out a medical radiation exposure survey involving both public and private medical institutions in the period of 2007 to 2009 to develop DRLs in diagnostic radiology, dental radiology and diagnostic nuclear medicine. This survey obtained qualitative and quantitative information on the frequencies and doses for diagnostic procedures. The establishment of DRLs as part of the optimization process are set on the basis of measured dose levels for average size patients in medical institutions at national level and compare with regional or local levels. If DRLs are consistently exceeded, the relevant medical institutions have to reviewed to determine whether radiation protection has been optimised. The development of DRLs circular has been reviewed by National Coordinators (MOH) from various disciplines together with other specialists from the private sectors and the universities. This Director General of Health circular can be access in the official website of Radiation Health and Safety Section, Engineering Services Division at https://radia.moh.gov.my/
Radiation Quantities
To understand the DRLs values, patients or radiation workers need to understand the radiation quantities that are involved in patient dosimetry. The radiation quantities are basically divided into three categories, namely, source quantities, field quantities and patient dose quantities, as shown in Figure 2. Patient dose quantities are calculated based on the exposure parameters. The medical physicist can help the patients to calculate the dose that they received during the diagnostic procedures.
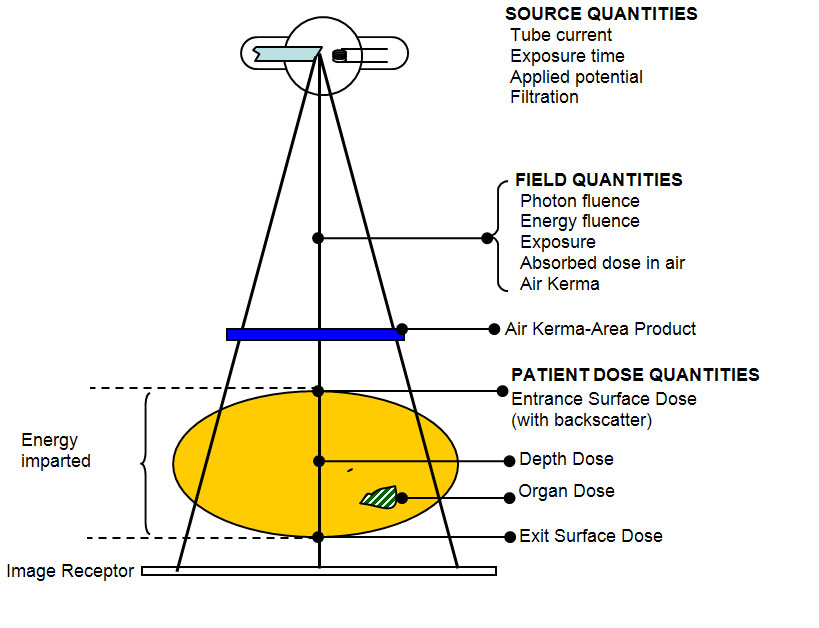
Figure 2: Radiation quantities
References
- Atomic Energy Licensing Act 1984 (Act 304)
- Atomic Energy Licensing (Basic Safety Radiation Protection – BSRP) Regulations 2010
- Jerrold T. Bushberg. 2002. The Essential Physics of Medical Imaging. Lippincott Williams & Wilkins.
- Richard R. Carlton, Arlene M. Adler. 2006. Principles of Radiographic Imaging: An Art and a Science, 4th ed. Thomson Delmar Learning.
- Colin J. Martin, David G. Sutton. 2002. Practical Radiation Protection in Healthcare. Oxford University Press.
- http://www.sprawls.org/
| Last Reviewed | : | 8 October 2014 |
| Writer / Translator | : | Nurmazaina bt. Mat Ariffin |
| Accreditor | : | Nik Mohamed Hazmi b. Nik Hussain |







