Introduction
Semen analysis is usually performed to help determine why a couple is having difficulty conceiving, as it is the easiest screening to evaluate male fertility. SFA is also performed to follow the course of a treatment affecting testicular or accessory gland function, or following vasectomy. Despite this important initial screening, many men experience anxiety over the test and later, over the results.
Repetition of at least two SFA is a critical component to achieve an accurate diagnosis. There may be a significant variation between semen parameters in different samples from a given patient. Stress over the test, trouble producing a sample for the analysis, and the medications currently taken could also led to inaccurate SFA result.
It is preferable that the samples are collected over more than one spermatogenic cycle (two months), particularly if a recent insult to spermatogenesis such as viral illness or gonadotoxin exposure has occurred. Abnormal results after appropriate repetition of SFA would be concluded as male factor infertility. It is reported that male factor infertility contributes for 20% to 40% of the infertility cases in United States alone.
Good sampling procedure
Each sample should be collected after an ejaculatory abstinence period of 2 to 5 days. Male patient produces sample by either masturbation, sex with a condom, sex with withdrawal before ejaculation, electric stimulation or anal stimulation with the first method being widely used in Malaysia.
Samples should be collected in wide-mouthed, sterile containers and maintained as close as possible to body temperature. The sample has to reach the laboratory within 20 minutes and analyzed within 1 hour in order to get a good sampling. The semen sample is then allowed to liquefy and is examined under light microscopy.
Parameters to be analysed
Freshly ejaculated semen is a gray-opalescent, semisolid coagulum that should spontaneously liquefy within 15 to 60 minutes. Semen that is red or yellow may indicate hematospermia or jaundice. Abnormalities of liquefaction and viscosity may indicate the presence of infection, defects in prostatic proteolytic enzymes, or absence of the seminal vesicle or prostatic components.
The main parameters analyzed are ejaculate volume, pH, sperm concentration, total sperm number, sperm motility, and sperm morphology. The normal values of these parameters are summarized in the table below.
It is critical to recognize that these semen parameters do not reflect ‘‘normal’’ or ‘‘average (mean)’’ values, but a reflection of an attempt to identify minimum values, below which, men are at high risk of contributing to infertility in a couple.
Table 1: Reference Values for Semen Analysis parameters Published by the World Health Organization (WHO) in 2010
|
Parameters |
2010 WHO reference value |
|
Semen volume |
?1.5 mL |
|
pH |
7.2-8.0 |
|
Sperm concentration |
?39×106 per ejaculate |
|
Total sperm number |
?15×106 per mL |
|
Total motility |
?40% |
|
Progressive motility |
?32% |
|
Sperm morphology |
?4% normal forms by strict criteria |
Recommended lifestyle
Listed below are the recommended lifestyle measures for male patients:
-
Healthy, balanced diet, high in green vegetables and fruits.
-
Stop smoking completely and avoid smoky atmosphere (passive smoking).
-
Reduce alcohol to a minimum (less than 5 units a week).
-
Avoid other recreational drugs.
-
Wear loose boxer-style underwear and avoid hot baths and hot environments.
-
Avoid sitting/driving for long periods. Try to take hourly breaks- 2 hours of driving heats scrotum (and testicles) by 2ºC.
-
Take vitamin A, C, E and minerals Zinc and Selenium (recommended daily allowance. Up to 1000mg a day for vitamin C).
-
Avoid exposure to noxious chemicals such as organic solvents and organophosphate pesticides.
-
Reduce stress.
Conclusions
The SFA functions as both a screening test for the presence of male factor infertility and as the cornerstone of the male factor evaluation. When the SFA is abnormal, further evaluation of the male will be indicated by the specialist.
Appendices:

Figure 1 : Assessing sperm morphology using CASA system
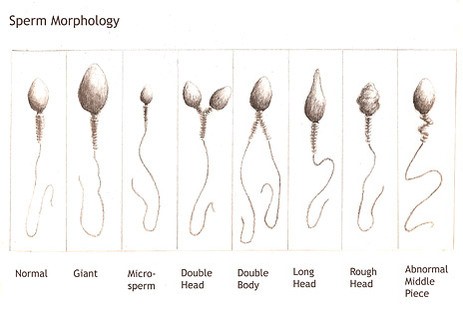
Figure 2 : Sperm morphology classification
References:
Cooper, T.G., Noonan, E., Eckardstein, S.V., Auger, J., Baker, H.W.G., Behre, H.M., et al. (2010). World Health Organization reference values for human semen characteristics Human Reproduction Update, Vol.16, No.3, 231–245.
Stahl, P.J., Stember, D.S.., and Schlegel, P.N. (2011). Interpretation of the Semen Analysis and Initial Male Factor. Management Clinical Obstetrics And Gynecology, 54, Number 4, 656–665.
Stephen, E.H., and Chandra, A. (2006). Declining estimatesof infertility in the United states: 1982-2002. Fertil Steril, 86, 516-523.
WHO laboratory manual for the examination and processing of human semen, WHO, 5th edition, 2010.
|
Last Reviewed |
: |
10 Mac 2015 |
|
Writer |
: |
Krishnan a/l Kanniah |
|
Translator |
: |
Krishnan a/l Kanniah |
|
Accreditor |
: |
Zamri bin Ahmad Yusof |







