Definition
Sperm cryopreservation (commonly called sperm banking or sperm freezing) is a procedure to preserve sperm cells. Sperm Cryopreservation is available for men who wish to bank sperm for future use. In Hospital Kuala Lumpur, sperm cryopreservation is done for Oncology patient, Neurology patient, as a back up for Assisted Reproductive Treatment (ART) backup and for men with severe oligospermia (sperm count less than 5×106/ml) who wish to do ART.
Background
In 1949, A.S. Parkes and two British scientists developed a method of using a syrupy substance known as glycerol to protect semen from injury during freezing. The process was further refined in 1953 by Dr. Jerome K. Sherman, an American pioneer in sperm freezing. Sherman introduced a simple method of preserving human sperm using glycerol, combined with a slow cooling of sperm, and used solid carbon dioxide as a refrigerant. Sherman also demonstrated for the first time that thawed sperm were able to fertilize an oocyte and showed normal development. As a result of this research, the first successful human pregnancy with thawed sperm was reported in the same year. In 1988, Dr. J.K. Sherman, wrote a report on behalf of the American Association of Tissue Banks and Reproductive Council, reported 500 pregnancies using thawed sperm frozen.
Medical treatments such as cancer therapies can have a damaging effect on sperm quality. Patients are typically referred to the Andrology Laboratory for sperm cryopreservation by their clinician. Sperm cryopreservation allows future use of sperm in fertility treatments such as Intra Uterine Insemination (IUI) or In Vitro Fertilization (IVF) or Intracytoplasmic Sperm Injection (ICSI). Frozen sperm can be used almost indefinitely after cryopreservation. The longest reported duration resulting in a successful pregnancy using cryopreserved sperm is 22 years.
Methodology
A short consultation will be given to the patients giving them an opportunity to ask questions and clarify details .After signing the Semen Storage Consent Agreement patients are screened for HIV, Hepatitis or other sexually transmitted diseases (STD).
Sperm is frozen using either a controlled-rate, slow-cooling method (slow programmable freezing or SPF) or a newer flash-freezing process known as vitrification. Vitrification gives superior post-thaw motility and cryosurvival than slow programmable freezing (Vutyavanich et al., 2010).
After a semen sample has been collected, it is placed at room temperature to liquefy. After liquefaction, the semen sample is analyzed for sperm concentration and morphology. The semen sample is mixed in a 1:1 ratio with a freezing medium that allows the sperm to survive the freezing and storage process. The semen and freezing medium mixture is divided up into two milliliter portions and placed in special containers called cryovials. The freezing medium used contains cryoprotectants. Cryoprotectants are chemicals that help remove water molecules from the cells being frozen. If the water molecule is not removed from the sperm, ice crystals will form inside of the cell and break up it up, resulting in cell death.?Semen samples are slowly frozen in liquid nitrogen vapors. Once the samples have been frozen in the liquid nitrogen vapors, they are placed in special containers called Cryotank where they are stored in the liquid nitrogen until they are needed. Each vial of a patient’s semen sample is labeled with the patient’s name and identification number. For each step verification is done by Senior Embryologist or Andrologist.
Outcome
Freeze–thawing procedure has a detrimental effect on Deoxyribonucleic acid (DNA), morphology, membrane integrity, and vitality of sperm (Hammadeh et al., 2001). The survival rate of sperm after cryopreservation is highly variable depends on the parameters before being frozen. If one of semen parameter fell below 5% of the World Health Organization reference values, recovery of motile and viable spermatozoa after thawing was low (Selene et al.,2013). Usually, after thaw, 50% of sperm will lose their motility (Verheyen et al., 1993).
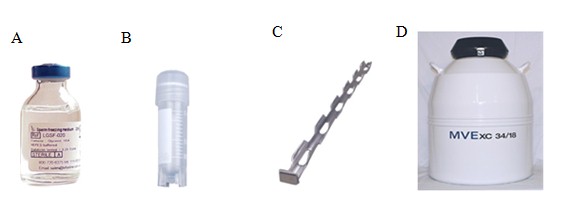
Figure: (A) Sperm freezing media containing cryoprotectant (B) Cryovials a container containing mixture of sperm and cryoprotectant (C) Cryocane used to hold cryovials during storage (D) Cryotank containing liquid nitrogen used for sperm cryopreservation
Reference:
- Hammadeh M. E., Szarvasy D., Zeginiadou T., Rosenbaum P., Georg T., Schmidt W. Andrology: Evaluation of Cryoinjury of Spermatozoa After Slow (Programmed Biological Freezer) or Rapid (Liquid Nitrogen Vapour) Freeze–Thawing Techniques. Journal of Assisted Reproduction and Genetics . 2001. Vol. 18, Issue 7, pp 364-370
- Kiran P. Nallella, Rakesh K. Sharma,Shyam S. R. Allamaneni, Nabil Aziz,and Ashok Agarwal. Cryopreservation of human spermatozoa: comparison of two cryopreservation methods and three cryoprotectants. Fertility and Sterility. 2004. Vol. 82, No. 4.
- World Health Organization. WHO Laboratory Manual For The Examination & Processing Of Human Semen. 2010. 5th Edn.271p.
| Last reviewed | : | 10 Mac 2015 |
| Writer | : | Krishnan a/l Kanniah |
| Translator | : | Krishnan a/l Kanniah |
| Accreditor | : | Dr.Kannapan a/l Palaniappan |







