Introduction
Congenital heart defects refer to malformation of the heart and the large vessels which are present at birth. About 8 to 10 in every 1000 babies are born with congenital heart defects. In many cases, the heart defects are relatively mild and do not require any treatment. For children with significant heart lesions, they may need medication or heart surgery. Certain heart defects can be treated by specialized procedures performed at cardiac catheterization laboratory (Figure 1) which are known as transcatheter treatment.

Figure 1: Cardiac catheterization laboratory
Transcatheter treatment involves the insertion of a thin flexible tube called a catheter, which is threaded from a vessel in the groin into the heart (Figure 2). This catheter, together with a wire, can be placed in different sites in the heart or vessels guided by live X-ray imaging. Once in position, an expanding plug or device may be placed to seal a hole or block off an abnormal or unwanted blood vessel. Alternatively, an inflatable balloon can be used to stretch open a narrow valve or blood vessel.

Figure 2: Insertion of a sheath through a vessel
in the groin before a catheter
Some of the commonly performed procedures include:
- Transcatheter closure of patent ductus arteriosus (PDA)
- Transcatheter closure of atrial septal defect (ASD)
- Transcatheter closure of ventricular septal defect (VSD)
- Balloon dilation to open narrowed pulmonary valve or pulmonary stenosis (PS)
- Balloon dilation to open narrowed aorta or coarctation of the aorta (CoA)
Before describing the procedures in details, it is important to understand the structure of a normal heart and how it works.
The normal heart
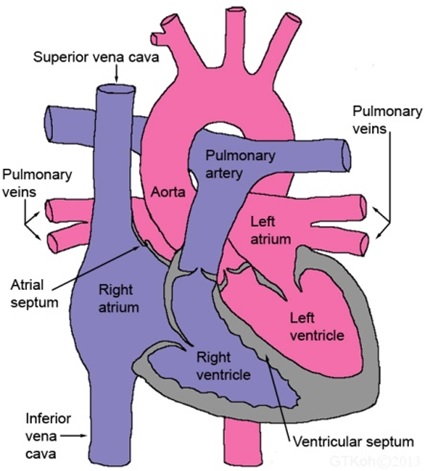
Figure 3: Normal heart
The normal heart consists of four pumping chambers. The two upper chambers are termed as right and left atrium. These two chambers are separated by a wall called the atrial septum. The two lower larger chambers are the right and left ventricles which are separated by a partition called the ventricle septum (Figure 3).
The oxygen-poor blood from the body fills the right atrium through two main veins, namely the superior vena cava and the inferior vena cava. From the right atrium, the blood flows to the right ventricle.
The right ventricle pumps the oxygen-poor blood through the pulmonary artery to the lungs to replenish oxygen. Now, the oxygen-rich blood from the lungs flows to the left atrium through the pulmonary veins. From left atrium, the blood flows to left ventricle and subsequently will be delivered to the whole body via the aorta
Transcatheter closure of patent ductus arteriosus (PDA)
 |
 |
 |
| Figure 4: PDA | Figure 4A: PDA device | Figure 4B: PDA coil |
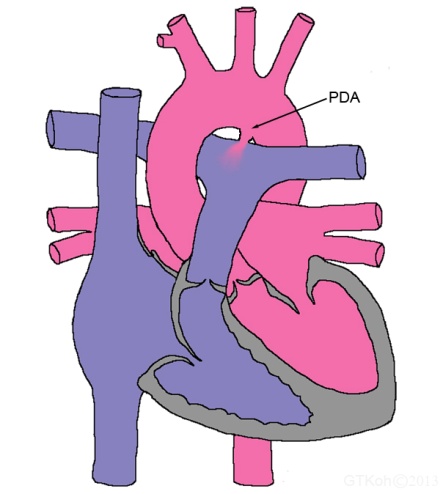
Ductus arteriosus is a blood vessel that connects the two main arteries of the heart, namely the aorta and the pulmonary artery (Figure 4). It is a normal structure in a baby’s heart prior to birth. It usually closes by itself within hours or days after birth.
Sometimes the ductus arteriosus fails to close on its own accord and remains open or “patent”. This condition is called patent ductus arteriosus or PDA in short. It is also known as persistent arterial duct.
A moderate or large PDA, if left untreated over a period time, may eventually lead to permanent damage to the heart and lungs. If the PDA is small, there is very little risk of damaging the heart or lungs, however, there is still a risk of infection of the lining of the heart or valves. This infective condition is called bacterial endocarditis. So it is recommended that even small PDA should be closed.
Closure of PDA can be done by transcatheter technique or surgery. Nowadays, most PDAs are treated by transcatheter technique with the exception of very small infant, very large PDA and unusual PDA structure or shape.
Procedural methods:
- Your child will be given a general anaesthesia or deep sedation. During anaesthesia, a breathing tube is placed in your child’s windpipe (trachea).
- A thin flexible tube called a catheter will be inserted into a vein in the groin.
- X-rays are used to guide the catheter to the correct position in the heart.
- Contrast dye is injected through the catheter for a clearer visual of the duct via X-ray.
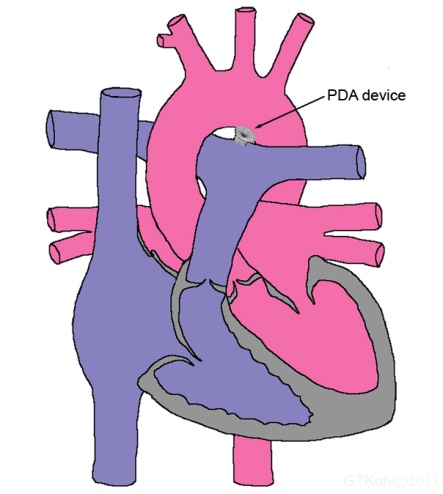
- Once the catheter is in the correct position, a small device or plug is threaded along the catheter and deployed inside the duct to close it (Figure 4A).
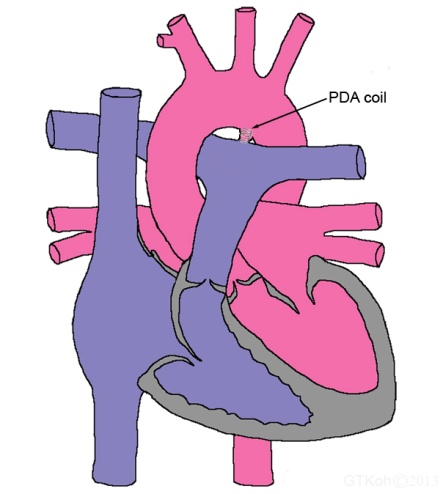
- If the PDA is very small, a small stainless steel coil (like a spring) is placed inside the duct instead (Figure 4B).
- The catheter will then be removed.
- Both the device and the coil are designed to stay in position and will stay in place throughout your child’s life.
Transcatheter closure of atrial septal defect (ASD)
 |
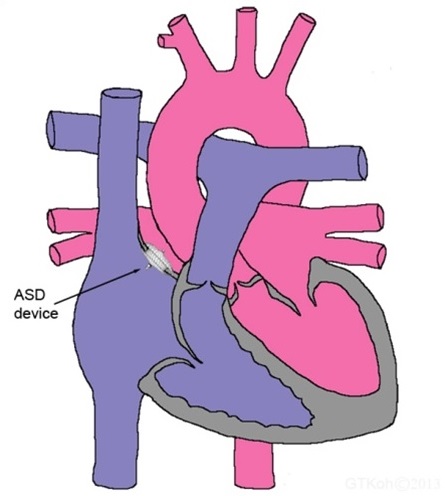 |
| Figure 5: ASD | Figure 5A: ASD device |
An atrial septal defect is a hole between the dividing wall of the two upper pumping chambers (atriums) of the heart (Figure 5). The defect allows blood from the left atrium to pass to the right atrium and therefore causes greater amount of blood to enter the right side of the heart and lungs. As a result, the right side of the heart is enlarged and the pressure in the lung vessels is increased. A moderate or large ASD, if left untreated over a period time, may cause permanent damage to the heart and lungs.
Closure of ASD can be achieved by transcatheter technique or surgery. At present, most ASDs are treated by transcatheter technique with the exception of large ASD in small infants and certain types of ASD.
Procedural methods:
- Your child will be given a general anaesthesia. During anaesthesia, a breathing tube is placed in your child’s windpipe (trachea).
- A small tube will be inserted into your child’s food pipe (oesophagus) through their mouth.
- This tube (transoesophageal echocardiography) is for scanning the heart to see the ASD more clearly and to measure the defect size.
- A catheter will be inserted into a vein in the groin.
- X-rays are used to guide the catheter to the right position in the heart.
- Once the catheter is in place, a device is folded up and pushed through the catheter and once it is out of the catheter, the device will unfold like an umbrella.
- The device which consists of two discs made with wire frames sewn together will then “sandwich” the defect (Figure 5A).
- The catheter will then be removed.
- The device is designed to stay in position and will stay in place for the rest of your child’s life.
Transcatheter closure of ventricular septal defect (VSD)
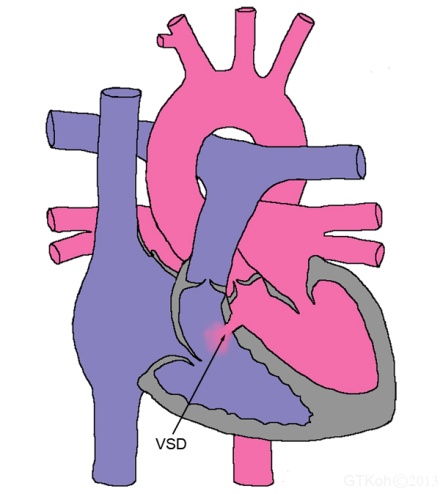 |
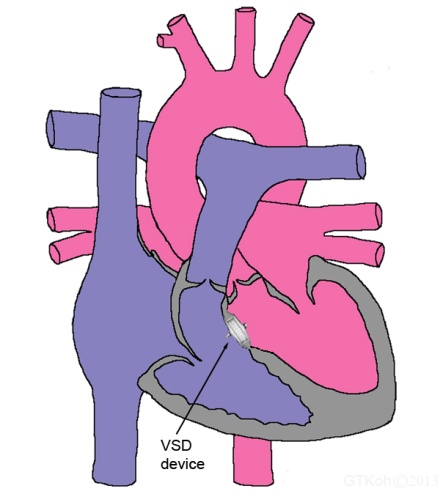 |
| Figure 6: VSD | Figure 6A: VSD device |
A ventricular septal defect is a hole in the ventricular septum, which is the wall between the lower pumping chambers (ventricles) of the heart (Figure 6). The defect can occur in any part of the ventricular septum. A VSD may be small or large, and sometimes there may be multiple defects. The defect grants passage for the blood from the left ventricle to flow to the right ventricle. This causes abnormal amount of blood to enter the lungs. Hence, the left side of the heart is dilated and the pressure in the lung vessels is elevated. Without treatment, a moderate or large VSD may result in permanent impairment to the heart and lungs.
Most VSDs are closed surgically but a subgroup of patients can be closed by transcatheter technique.
Procedural methods:
The transcatheter procedure is more or less similar to technique used for ASD, however it is technically more difficult and complex. The device used for VSD is different from ASD but the design is conceptually the same, having two discs of wire frames to seal the defect (Figure 6A).
Balloon dilation to open narrowed pulmonary valve or pulmonary stenosis (PS)
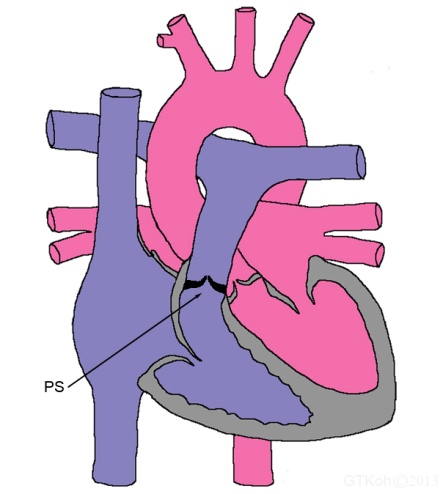 |
 |
 |
| Figure 7: Pulmonary stenosis | Figure 7A: Balloon dilation | Figure 7B: Valve opened |
Pulmonary stenosis refers to narrowing of the pulmonary valve (Figure 7). The heart contains four valves. These valves open and close to maintain blood flowing forward through the heart and vessels. The pulmonary valve is located between the right lower pumping chamber (right ventricle) and blood vessel to the lungs (pulmonary artery). Due to the narrowing of the valve, the blood flow to the lungs is obstructed.
The muscle of the right ventricle has to work harder to compensate for this narrowing. This causes the right ventricle to thicken or enlarged and unable to pump blood efficiently. In some rare cases, severe pulmonary stenosis can even cause death if it is not treated. Most children have only mild pulmonary stenosis and do not need any treatment at all.
For those who require treatment, the mainstay of treatment is by transcatheter technique with the exception of those with severely deformed valve or the obstruction is below or above the valve. For this group of patients with severe cases, the option is to repair or replace the valve or remove obstruction by surgery.
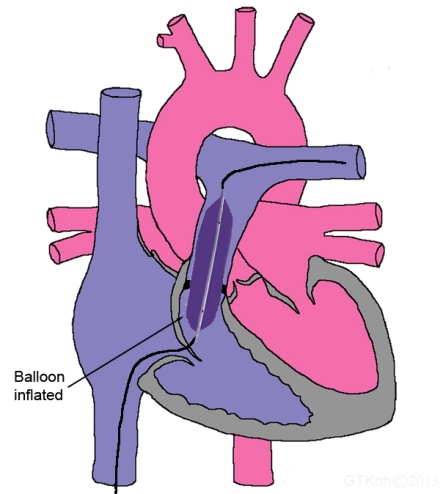
Procedural methods:
- Your child will be given a general anaesthesia. During anaesthesia, a breathing tube is placed in your child’s windpipe (trachea).
- A catheter will be inserted into a vein in the groin.
- X-rays are used to guide the catheter to the correct location in the heart.
- Contrast dye maybe injected through the catheter for better X-ray clarity.
- Once the catheter with wire is in the correct position, the catheter is removed and exchanged with a small collapsed balloon.
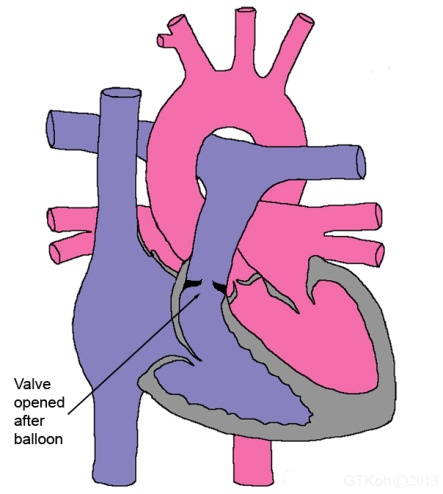
- The balloon is placed in the narrowed valve and gently inflated, stretching the valve open (Figure 7A).
- The balloon is then deflated and removed with the wire (Figure 7B).
Balloon dilation to open narrowed aorta or coarctation of the aorta (CoA)
 |
 |
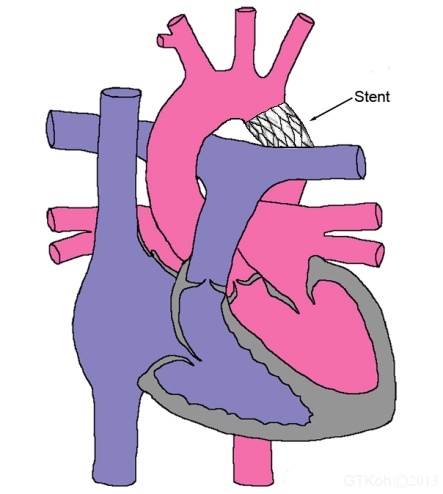 |
| Figure: CoA | Figure 8A: Balloon inflation | Figure 8B: CoA stenting |
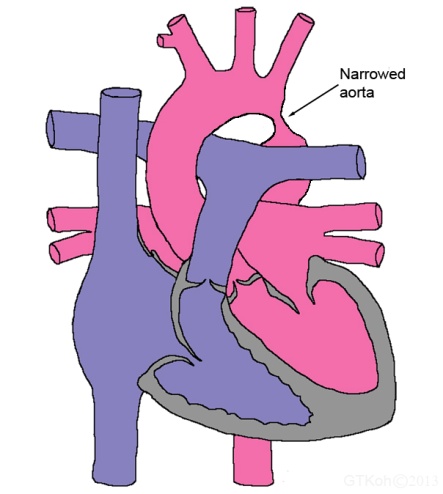
Coarctation of the aorta (CoA) is a narrowing of the aorta usually occurs just beyond the branches that supply the head and arms with blood (Figure 8). The aorta is the large blood vessel that carries blood from the heart to the rest of the body. The narrowing prevents the blood from circulating normally in the lower half of the body. CoA can gradually worsen the heart function if untreated.
This condition can be treated by surgical repair or transcatheter technique. Transcatheter treatment is more suited for older children and with discrete narrowing.
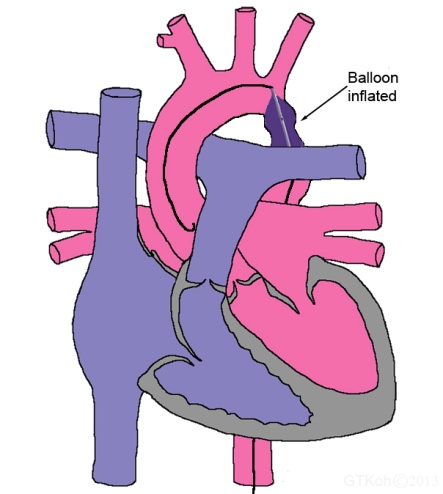
Procedural methods:
- Your child will be given a general anaesthesia. During anaesthesia, a breathing tube is placed in your child’s windpipe (trachea).
- A catheter will be inserted into an artery in the groin.
- X-rays are used to guide the catheter to the exact location in the aorta.
- Contrast dye maybe injected through the catheter for a clearer view of the narrowing on X-rays.
- Once the catheter with wire is in the correct position, the catheter is removed and exchanged with a small collapsed balloon.
- The balloon is positioned in the narrowed aorta and gently inflated to widen the narrowing (Figure 8A). This is known as
- The balloon is then deflated.
- In older children especially after puberty, a stent (an expandable metal mesh tube) may be inserted to keep the narrowed aorta open (Figure 8B).
Pro and cons of transcatheter treatment
The major advantage of transcatheter treatment compared to surgical repair is its relative non-invasive approach. Most patients do not need specialized care in intensive care unit after the procedure. Patients who have undergone the procedure can usually be discharged the next day and many return to school or work within 1-2 days. The puncture site in the groin will usually heal well without scarring.
The major disadvantage of this treatment is that only selected heart lesions that can be treated this way. As this form of treatment is relatively new compared to surgery, there is a paucity of long term outcome data.
Complications or risks
Transcatheter treatment is usually very successful and carries a very low risk. Almost all children will survive without any major complications. The complications can be categorized into general complications and specific complications. General complications are applicable to all transcatheter treatment, while specific complications are relevant to the specific procedure by itself.
General complications
Some patients may develop reaction to the sedative and anaesthesia medications, however this is not common.
There is a small risk of developing allergic reaction to the contrast dye. The risk is higher in patientswith history of allergy.
There is a minimal risk of bleeding from the puncture site. Generally, simple manual compression is sufficient to control the bleeding.
There is a risk of injury to heart or blood vessels by the catheters and wires but the risk is very low.
Specific complications
Transcatheter closure of patent ductus arteriosus (PDA)
There is a small risk that the closure device or coil will not completely close the duct. Sometimes complete closure can only be achieved after a few months. If it does not close on its own, it is usually necessary to repeat the treatment.
There is a very slight risk that the closure device may move out of position. It is usually possible to retrieve it using transcatheter technique. If this fails, then your child may need surgery to remove the device.
The device may become infected but this is extremely rare. However, this is a very serious complication and will require surgery to retrieve the device.
Transcatheter closure of atrial septal defect (ASD)
There is a low risk that the closure device will not completely close the defect. Most patients will have complete closure after a few months. If the residual defect is significant, your child may need another procedure or surgery to close the defect.
There is a minimal risk that the closure device may move out of position. It may be possible to retrieve it using transcatheter technique. If this fails, your child may need surgery to remove the device and close the defect.
The device may become infected but this is very rare. Your child will require antibiotic treatment and surgery to take out the device.
There is also a very unlikely risk of blood clots forming on the device surface or inside the heart which could cause a stroke.
Transcatheter closure of ventricular septal defect (VSD)
The risks are similar to transcatheter closure of ASD. However, there is a small risk that your child may develop complete heart block or third-degree AV heart block. In this condition, the electrical impulses from the atriums cannot be transmitted to ventricles. This is a serious complication and can lead to very slow heart rate and fainting episode. If this complication occurs, your child will usually need an implantation of a permanent pacemaker.
Balloon dilation to open narrowed pulmonary valve or pulmonary stenosis (PS)
There is a low risk that the balloon dilatation will not open the valve as desired especially for severely deformed or thickened valve. In that case, your child will usually need surgical repair.
Sometimes the dilatation will cause damage to the pulmonary valve and become leaky. Leaking through the valve is also called valve regurgitation. A small “leak” is common and unlikely to cause problems.
Balloon dilation to open narrowed aorta or coarctation of the aorta (CoA)
There is a slight risk that the balloon failed to open the narrowed segment of the aorta. If failed, your child will usually require surgical repair.
Sometimes despite successful dilation, the narrowing will redevelop with time. It is usually necessary to repeat the balloon dilation for this type of case.
There is a low risk of developing aneurysm (a weakened aortic wall which bulges out like a balloon) which might lead to aortic wall rupture.
There is a very small risk of getting stroke during the procedure.
| Last Reviewed | : | 29 June 2016 |
| Writer | : | Dr. Koh Ghee Tiong |
| Accreditor | : | Dr. Sharifah Ainon bt. Ismail Mokhtar |







