Introduction
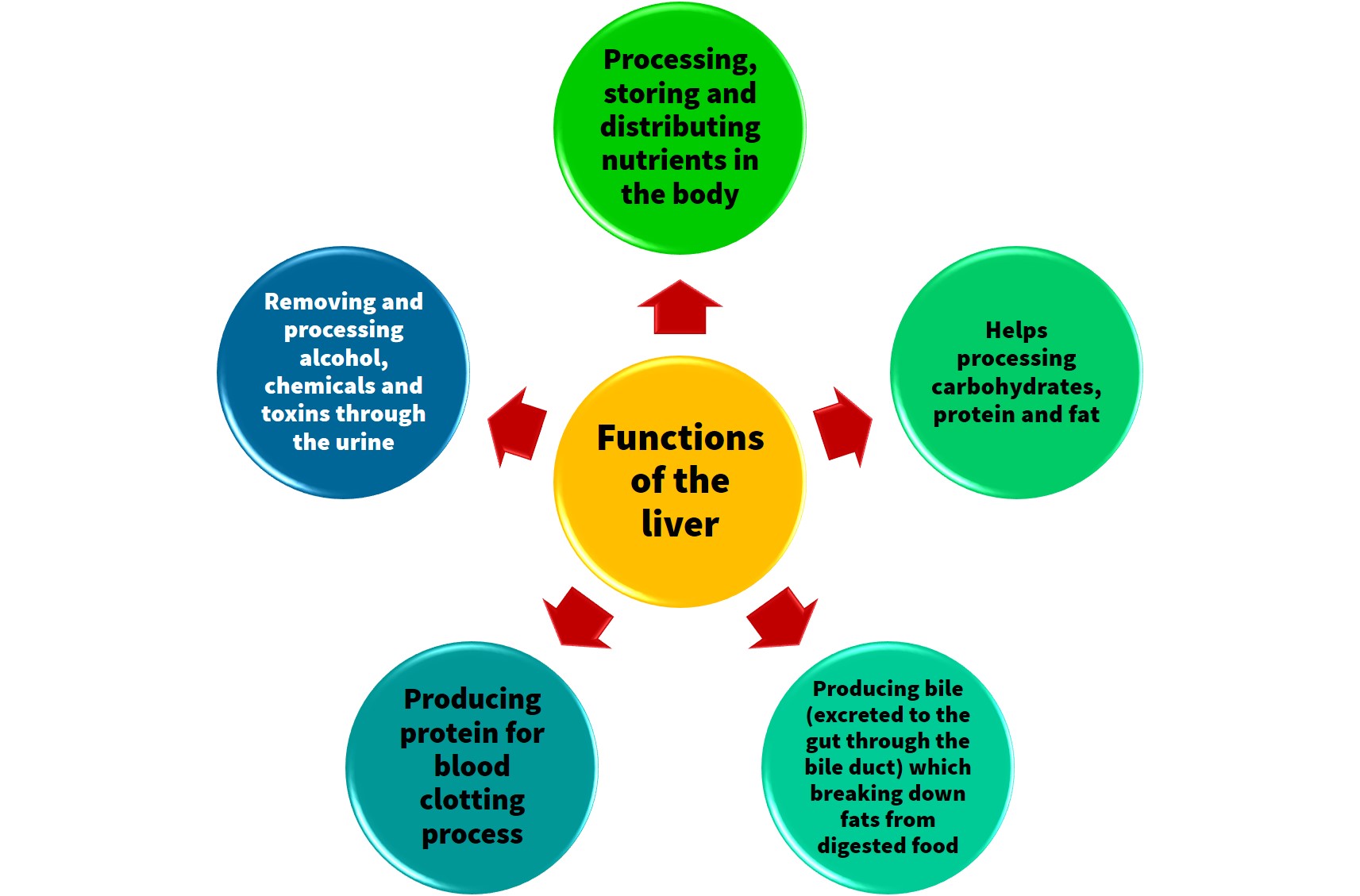
Liver is the most active organ in the body. It is located in the upper right abdomen.
Definition of Fatty Liver
Fatty liver is the result of the accumulation of excess fat in the liver. It is a common illness and most sufferers do not have symptoms and complications.
However, if it is not treated, the accumulated fat can cause inflammation and scarring to the liver, which can lead to liver failure.
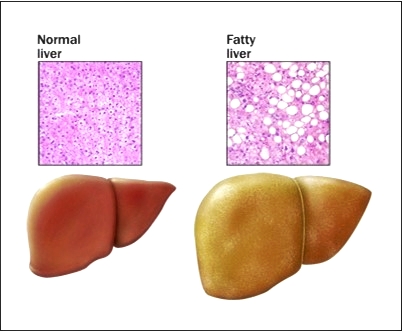
Figure 1 : Comparison between normal and fatty liver.
Compared to normal liver, fatty liver is enlarge and discoloured. Liver tissue shows an accumulation of fat.
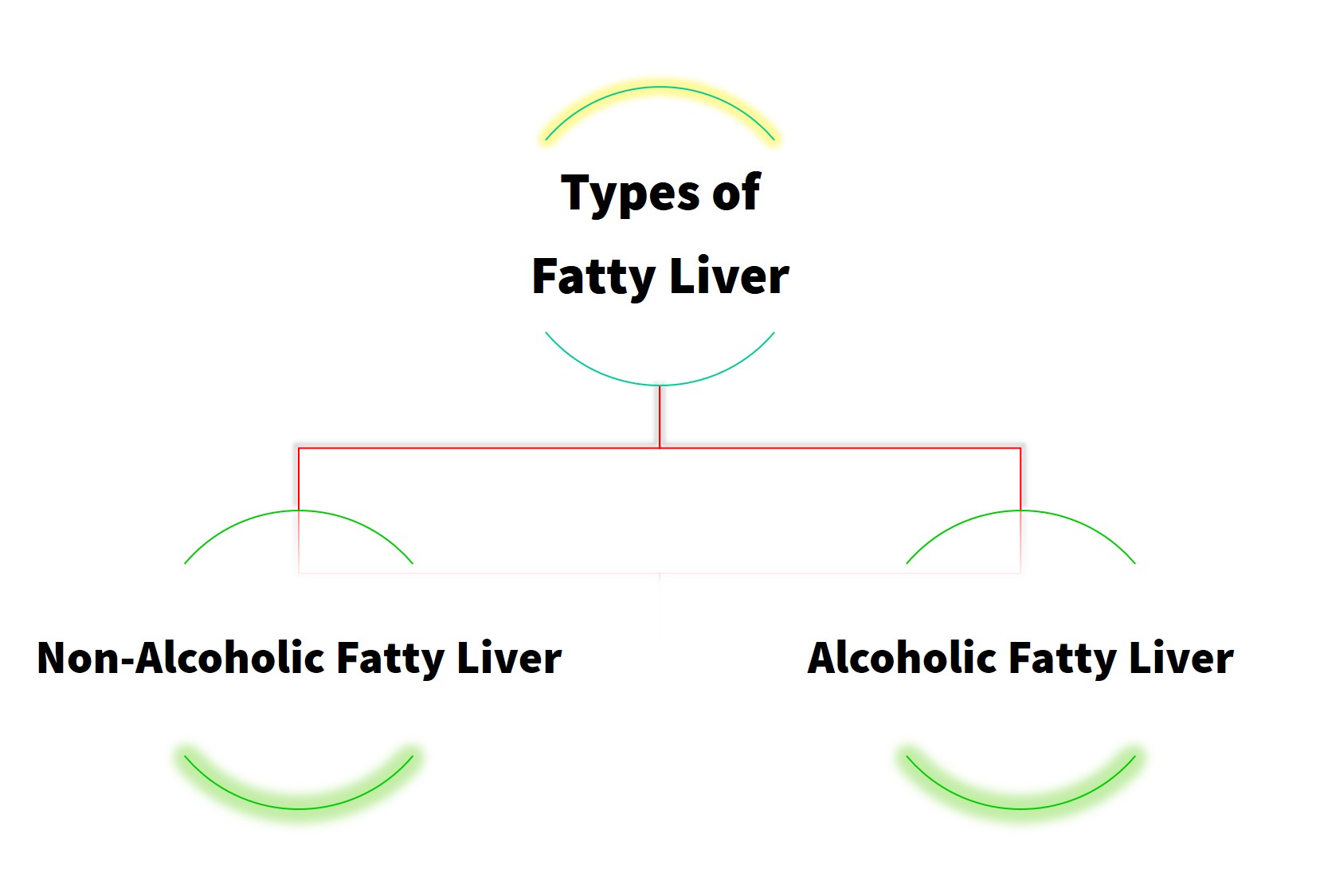
Types of Fatty Liver
- Non-alcoholic fatty liver
- It is caused by excessive alcohol use.
- People with fatty liver do not show any signs that they suffer from the disease.
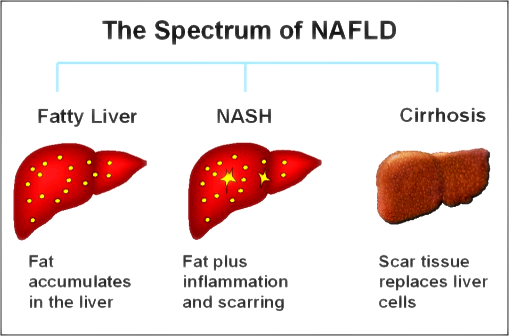
Figure 2 : Spectrum of non-alcoholic liver disease.
Causes of Non-Alcoholic Fatty Liver
Fatty liver happens resulting from imbalance fat production that is excessive and fat excretion that is low in the blood. As a result, the accumulation of fat occurs in the liver.
The causes are:
- Hypercholesterolaemia (high cholesterol in blood)
- Hypertriglyceridaemia (high triglyceride in blood)
- Metabolic syndrome – individual with more than 3 diseases, which are:
- Waist circumference for female greater than 80cm and for man more than 90cm
- Diabetes mellitus
- Hypertension
- Heart disease
- Obesity – Body Mass Index (BMI) more than 30kg/m2
- Diabetes mellitus.
- Alcoholic fatty liver
- It is caused by excessive alcohol use over a long period of time .
- Excessive alcohol intake for male is more than 4 cups per day.
- Excessive alcohol intake for female is more than 3 cups per day.
- Genetic factors may also cause alcoholic liver disease.
- Alcohol addiction is the main cause that affects the liver enzyme (ALT, ALP and AST) which involved in the metabolism of food in the liver.
- It is caused by excessive alcohol use over a long period of time .
Reference : Rosak Hatimu Akibat Arak
Symptoms of Fatty Liver
People with fatty liver disease usually do not realise on the symptoms the have. The symptoms are :
- Enlarged liver (Hepatomegaly)
- Discomfort at upper right abdomen
- Lethargy.
Laboratory Tests
Liver enzymes levels are used to diagnose fatty liver. Fatty liver is the main cause of liver enzymes levels in the blood becomes abnormal.
Liver enzymes are :
- Alkaline Phosphatase (ALP)
- Alanine Transaminase (ALT)
- Aspartate Transaminase (AST)
Other laboratory tests to determine the fatty liver are :
- Triglyceride
- LDL cholesterol
- HDL cholesterol
- total cholesterol, and
- blood glucose
The table below shows the normal levels for the tests that are used to diagnose fatty liver :
| Laboratories Test | Normal Level |
|---|---|
| Alanine Aminotransferase (ALT) |
Male : 0 – 40 U/L Female : 0 – 3 U/L |
| Alkaline Phosphatase (ALP) |
Male : 53 – 128 U/L Female : 42 – 98 U/L |
| Aspartate Transaminase (AST) |
Male : 0 – 40 U/L Female : 0 – 31 U/L |
|
Glucose test Fasting Blood Sugar (FBS) Randomised Blood Sugar (RBS) |
3.8 – 6.0 mmol/L 7.8 – 11.1mmol/L |
| Total Cholesterol (T Chol) | < 5.2mmol/L |
| LDL Cholesterol (LDL-C) | < 3.4 mmol/L |
| HDL Cholesterol (HDL-C) |
Male : 0.9 – 1.45mmol/L Female : 1.15 – 1.68 mmol/L |
| Triglyceride (TG) | < 2.3 mmo/L |
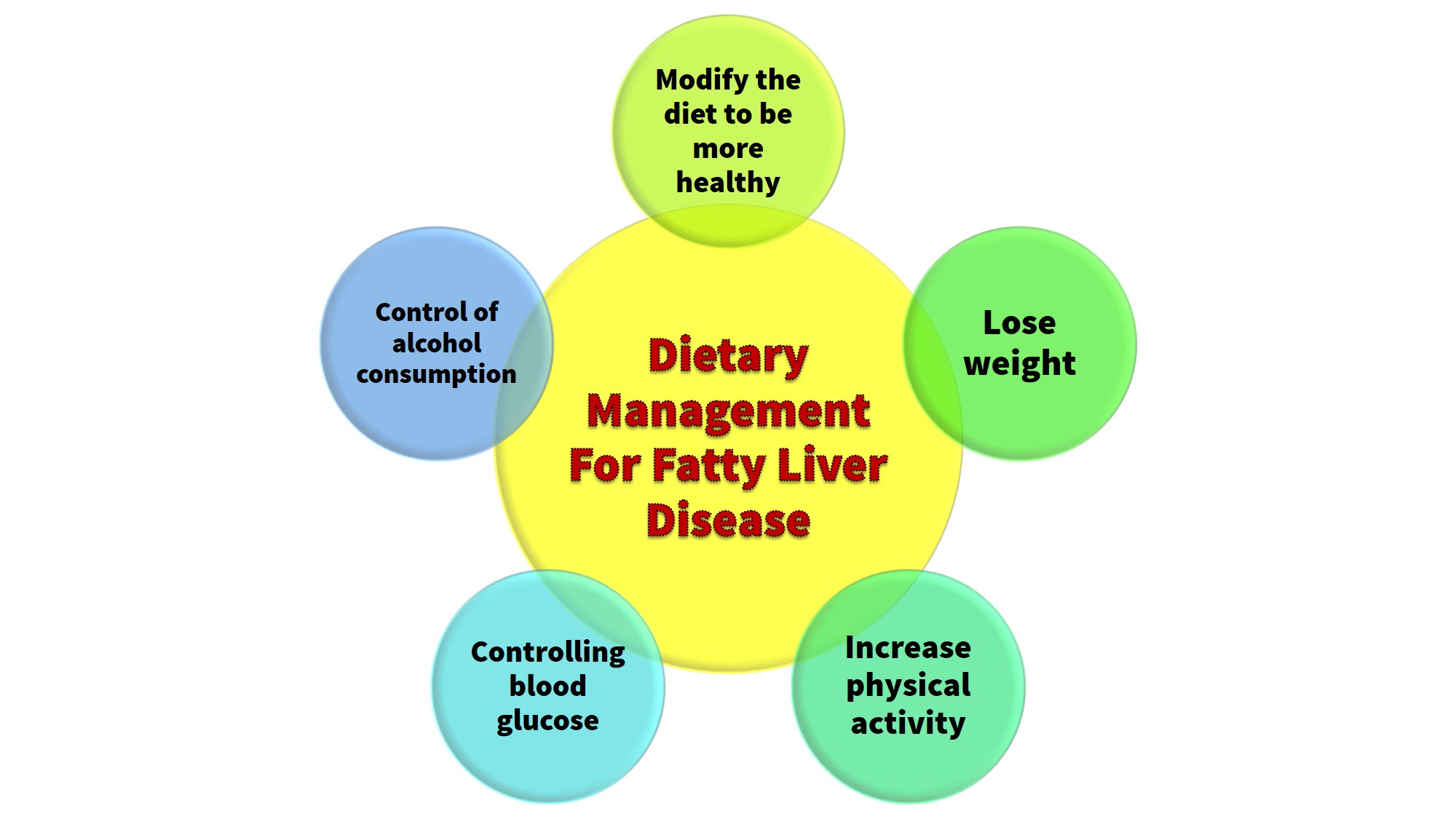
Dietary Management For Fatty Liver
Diet management therapy that is to be applied depends on the cause of the fatty liver.
For example, if the fatty liver disease is caused by high cholesterol in the blood, the diet control and physical activity can reduce the risk of fatty liver, heart disease or stroke.
-
- Modify the diet to be healthier
- Lifestyle modification includes consuming a healthy diet, which is to reduce the intake of high fat and high cholesterol foods, and increase fibre intake such as vegetables and fruits. This can help in reducing fat in the liver.
Reference : Diet For Hypercholesterolaemia
- Lifestyle modification includes consuming a healthy diet, which is to reduce the intake of high fat and high cholesterol foods, and increase fibre intake such as vegetables and fruits. This can help in reducing fat in the liver.
- Lose weight
- Fatty liver patients who are obese or overweight are encouraged to lose weight gradually.
- The recommended weight loss is between 3 to 10 % from current weight. This can help reduce the amount of fat in the liver cells.
- For example, if the patient’s weight is 80 kg, the weight loss of 3 to 10 % is 2.4 kg to 8 kg from the current weight.
- Increase physical activity
- Individual with fatty liver is encouraged to exercise to help reduce weight, control cholesterol and blood sugar.
- Recommendation of exercise is 30 to 40 minutes for 3 to 4 times per week.
- Controlling blood glucose
- Controlling blood glucose is important especially for diabetes mellitus patients. Please comply to medical prescription and the instructions given by your doctor.
- Control of alcohol consumption
- For non-alcoholic fatty liver, limit alcohol intake and for alcoholic fatty liver, they required to stop consuming alcohol.
- Modify the diet to be healthier
Conclusion
Dietary management of fatty liver patients is dependent on the cause of the disease whether the problem is overweight, obesity, high blood cholesterol, metabolic syndrome, or excessive alcohol consumption.
Therefore, patients must adhere to a diet that has been prescribed to reduce fat in the liver tissue.
References
- Chalasani N., Younossi Z., Lavine JE. Et al (2012) .Diagnosis and Management of Non-Alcoholic Fatty Liver Disease: Practice Guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. Journal of the American Association for the Study of Liver Disease.
- Fatty liver Disease. Melalui internet: http://www.mayoclinic.org/diseases-conditions/nonalcoholic-fatty-liver-disease/basics/prevention/con-20027761
- Fatty liver Disease. Melalui internet: http://www.webmd.com/hepatitis/fatty-liver-disease
- Rolfer et al. (2000). Nutrition, Liver Disease and Gallstones. Understanding Normal and Clinical Nutrition. 7th Ed. Peter Marshall. Thompson Higher Education. 10 Davis Drive, Belmont, CA 94002-3098 USA.
- The difference between normal liver and fatty liver (Rajah 1). Melalui internet : http://www.mayoclinic.org/diseases-conditions/nonalcoholic-fatty-liver-disease/basics/prevention/con-20027761. 2 April 2014.
- The spectrum of NAFLD (Rajah 2). Melalui internet : http://www.precisionnutrition.com/lean-liver-with-low-carb
- Ueno T., Sugawara H., Sujako K. et al (1997). Therapeutic effects of restricted diet and exercise in obese patients with fatty liver. Vol. 27, Issue 1 (103-107). Journal of Hepatology.
| Last reviewed | : | 28 August 2020 |
| Writer | : | Faulina Khamisan |
| Accreditor | : | Cyril Sibon |
| Reviewer | : | Nik Mahani Binti Nik Mahmood |