Introduction
Recurrent implantation failure (RIF) means failure to achieve pregnancy after several attempts of IVF cycles with transfers of good quality embryos. It affects 10% of women and is a particularly distressing condition.
The failure to implant may be a consequence of embryo or uterine/endometrial factors and also multifactorial. Investigations should be carried out to ascertain whether there is any underlying cause of the condition.
Treatment offered should aim to improve embryo quality or endometrial receptivity.
Recurrent Implantation Failure (RIF)
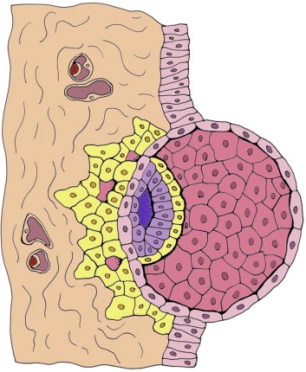
Figure 1.
The initial stage of implantation, when the embryo is invading the epithelial layer of the endometrium to be embedded in the stroma compartment.
Causes of recurrent implantation failures (RIF)
Embryo factors
Embryo factors still play a part in RIF because the currently used methods of embryo selection are not always reliable. Compromised oocyte quality is often suspected when there is a poor response to ovarian stimulation, low antral follicle count(AFC), high FSH and low anti-Mullerian hormone(AMH).
Poor-quality spermatozoa will also lead to the production of poor-quality embryos causing RIF. Other causes include zona hardening, suboptimal culture condition and suboptimal embryo transfer.
Uterine and Tubal factors
Congenital uterine anomalies may affect endometrial receptivity. The septate uterus is the most common structural uterine anomaly. Intracavity uterine pathologies including submucous fibroids, endometrial polyps and intrauterine adhesions may contribute to RIF.
Submucosal fibroids may distort the endometrial cavity and may cause decrease pregnancy and implantation rates. Pregnancy rates improve following the resection of fibroids distorting the uterine cavity. However, there is controversy as to whether non-cavity-distorting intramural fibroids adversely affect IVF outcome. Adenomyosis affects the junctional zone of the uterus which is just beneath the endometrium and so may have impact on implantation. Endometrial polyps may also interfere with embryo implantation. Intrauterine adhesions occurred in 8.5% of women with RIF.
Hydrosalpinx is a Greek word meaning a Fallopian tube filled with water or fluid. The adverse impact of hydrosalpinges on implantation may be attributed to a direct embryotoxic effect. There is good evidence that salpingectomy(removal of fallopian tubes) prior to IVF in women with hydrosalpinges improves outcome.
Other factors
Other factors which may contribute to RIF would include immunological factor and thrombophilic conditions.
Investigations for RIF
Women with RIF should be offered ovarian reserve tests such as basal FSH, AMH and AFC to exclude any significant compromise of ovarian function associated with RIF. Several laboratory tests are available to measure sperm DNA fragmentation. At present, sperm DNA integrity testing should only be offered to couples with RIF as part of a research programme. Karyotyping should be considered in couples with RIF.
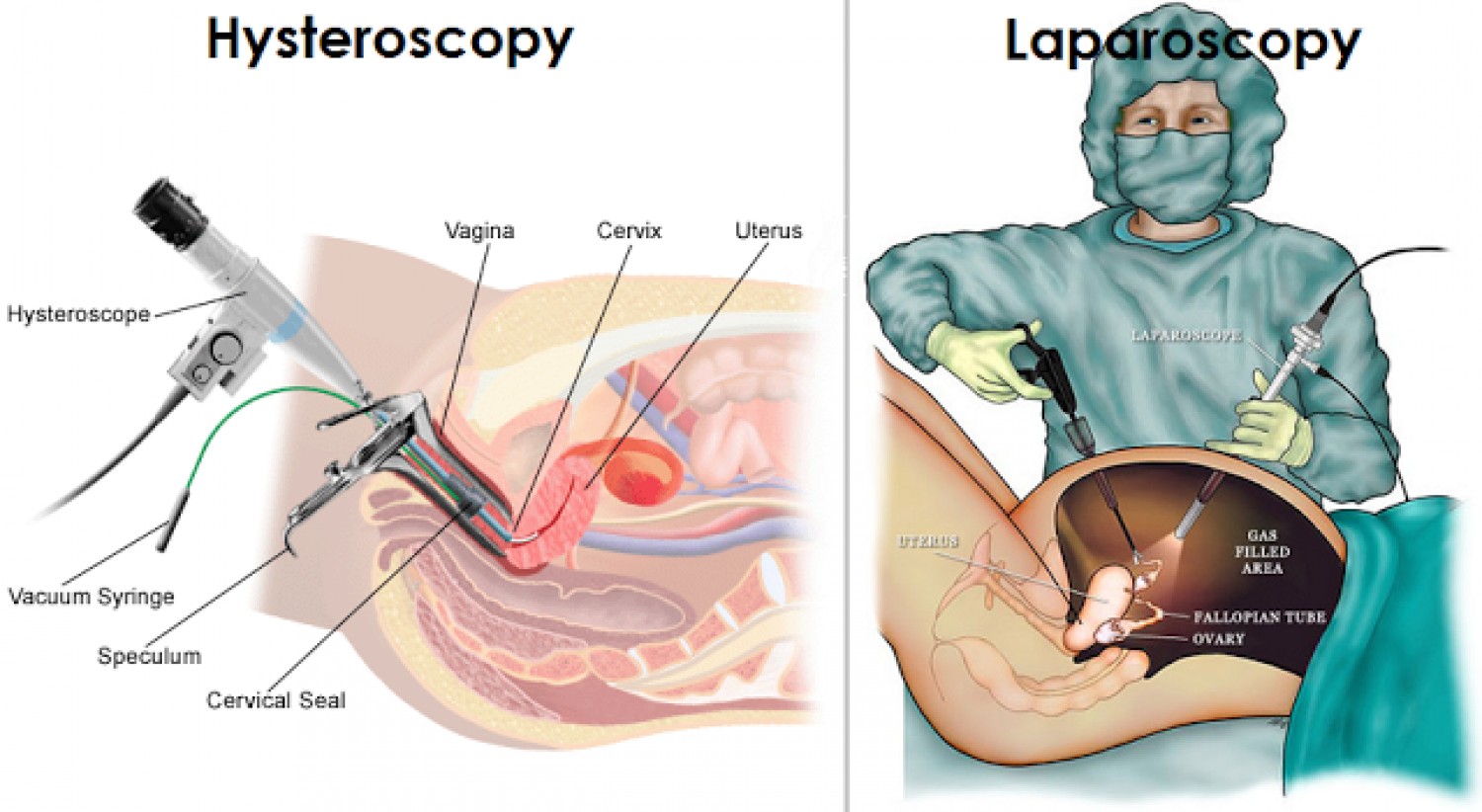
Ultrasound examination, hysterosalpingography(HSG), hysteroscopic and laparoscopic examination should be able to confirm or refute many diagnosis involving uterine/tubal pathology including fibroids, polyps,uterine septum, hydrosalpinx etc.
Management
Structural pathology
Any structural pathologies eg: uterine fibroids, uterine septum, endometrial polyp, hydrosalpinx etc. must be dealt with operative management accordingly.
Lifestyle changes
Lifestyle changes could improve the likelihood of treatment success. This include cessation of smoking and alcohol consumption, having normal BMI and anti-oxidant intake
Ovarian stimulation protocol
The ovarian response to gonadotrophin stimulation should be reviewed and gonadotrophin dose may be increased. Poor responders to FSH stimulation in down-regulated cycles may benefit from the addition of LH. In women with endometriosis and adenomyosis, the use of ultra-long protocol involving the administration of gonadotrophin-releasing hormone (GnRH) agonists for a few months prior to IVF or ICSI may increase the pregnancy rate.
Sperm DNA fragmentation
When suboptimal spermatozoa are considered to be a contributory cause of RIF, oral antioxidant may be used to improve sperm quality to reduce the incidence of sperm DNA fragmentation.
The use of testicular spermatozoa in RIF associated with high sperm DNA fragmentation in semen may increase in the pregnancy rate but further studies are required to confirm the benefit.
Embryos: issues related to RIF Improving embryo quality and selection
The implantation potential of a blastocyst is well recognized to be greater than that of the day-2 or -3 embryos and blastocyst transfer ought to be considered if not performed in previous treatment cycles.
Assisted hatching may be clinically useful in patients with a poor prognosis, including those with a history of two or more unsuccessful IVF cycles, poor embryo quality and older women (?38 years of age) and is worth considering in women with RIF.
To improve the embryo selection, metabolomic changes in the culture medium of embryos and oocytes (exometabolomics) may be measured determining what the embryo consumes or secretes (e.g. amino acids, proteins and oxygen consumption) and these parameters have been shown to correlate with embryo viability. Its application in women with RIF has yet to be confirmed.
The value of preimplantation genetic diagnosis (PGD) in RIF is controversial. There is no evidence to suggest that the embryos produced by women with RIF are more likely to be abnormal.
Embryo transfer: issues related to RIF
Embryo implantation has been found to be dependent on embryo quality, endometrial receptivity and transfer efficiency. In women with RIF, the details of previous embryo transfers should be reviewed, paying particular attention to any technical difficulties encountered. A trial embryo transfer should be considered where a prior embryo transfer has been described as difficult or where difficulty may be anticipated, such as previous cervical surgery.
Preliminary evidence to suggest that double sequential embryo transfer may be of benefit but carefully designed randomized controlled trials are required to confirm its value.
The transfer should be performed under ultrasound guidance because ultrasound-guided embryo transfer significantly increases the chance of conception.
There is insufficient evidence to show that bed rest after transfer improves outcome.
Endometrium: issues related to RIF
RIF may be associated with a thin endometrium (<7 mm) noted on the day of HCG administration or embryo transfer. Modified long protocol with exogenous oestrogen therapy started on second day menses and stopped on the day of HCG administration could address the issue of thin endometrium. Another treatment to increase endometrial thickness is sildenafil citrate. It is unclear whether luteal support with GnRHa has significant benefit over commonly used forms of luteal support eg: progesterone or HCG.
Endometrial scratch is of benefit in women with RIF but it should be carried out approximately 7 days prior to the onset of menstruation, immediately before the start of ovarian stimulation for IVF treatment.
Successful use of endometrial perfusion with granulocyte colony-stimulating factor in women who are resistant to oestrogen and vasodilators has been described but requires further investigation to confirm its usefulness.
Summary
Women with RIF should be offered appropriate investigations to rule out an underlying cause for the repeated failures. The main treatment strategy in couples with RIF is to improve the quality of the embryos transferred and the receptivity of the endometrium.
| Last Reviewed | : | 08 May 2017 |
| Writer | : | Dr. Roziana bt. Ramli |
| Accreditor | : | Dr. Wan Abu Bakar bin Yusuf |