What is a salivary gland calculus?
Salivary gland calculus, also known as salivary stone, is a calcified hard mass found within a salivary gland or salivary duct. Salivary calculus varies in sizes and may found in multiple numbers. A large calculus often cause blockage of salivary flow, resulting in accumulation of saliva within the gland, often described by patient as presence of pain and swelling at the affected area especially during eating.
Where does salivary gland calculus occur?
Salivary gland calculus mostly occurs in major salivary glands and its ducts. Our body has three pairs of major salivary glands namely parotid, submandibular and sublingual glands. Salivary duct is a pipe-like structure that allows the flowing of saliva produced by salivary glands into the mouth. The opening of parotid gland duct is located at the inner part of cheek opposite the upper second molar tooth whereas the opening of submandibular and sublingual glands is located at the floor of mouth behind the lower front teeth. The incidence of salivary gland calculus is more common in submandibular glands and its duct, followed by parotid glands and sublingual glands.
Source: http://www.istanbulentcenter.com/y/Salivary-Glands-Problems-68.html
Why does salivary gland calculus occur?
The exact cause of salivary calculus formation is unknown. Although salivary calculus consists mainly of calcium, no relationship has been established between the calcium level in the body and salivary calculus formation. However, certain factors that reduce the production of saliva or increase its consistency may contribute to salivary calculus. These factors include dehydration, not eating enough food that results in less stimulation of saliva and certain types of medication that affect the production of saliva.
Signs and symptoms of salivary gland calculus
The signs and symptoms of presence of salivary calculus are as follow:
- Pain and swelling at the affected salivary gland region
- In the absence of an infection, pain and swelling usually occur during meal time. This is known as a ‘meal time syndrome’. Pain and swelling will often subside gradually after the meal time. The intensity of the pain may vary from mild to severe, depending on the severity of salivary flow blockage
- In the presence of an infection, severe pain and swelling will present throughout the day. Other signs of infection include fever, redness over the affected salivary gland region and foul smell/taste in the mouth.
- Hard mass can be felt if the salivary calculus is located near the duct opening or along the duct
- In the case of recurrent infection of the salivary gland secondary to the salivary calculus, the affected gland will be firm in consistency on touch.
- Reduced or an absence of salivary flow from the affected salivary gland duct.
Investigations
- Plain X-rays, such as the following, will show presence of radiopaque (whitish) mass.
- Lower occlusal view
- Orthopantomogram
- Lateral oblique view
- Sialography
- A cannula will be inserted into the duct of an affected salivary gland. A dye is then injected into the duct through the cannula followed by an X-ray to identify the location of the calculus.
- Sialoendoscopy
- This method can be used for both diagnosis and treatment of salivary gland calculus. For diagnosis, a thin tube with camera at its tip will be inserted into the duct of the affected salivary gland to identify the location of the calculus.
- Ultrasound
- Computer tomography(CT) scan
- Magnetic Resonance Imaging (MRI)
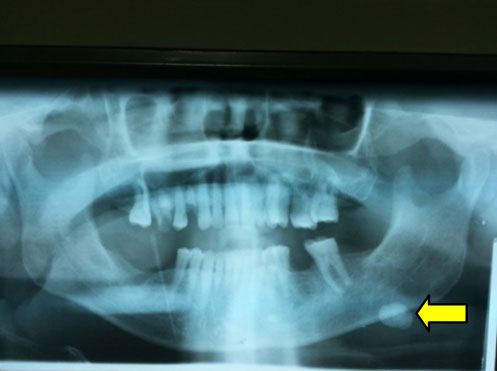
Orthopantomogram showing salivary calculus (arrow) at left jaw region
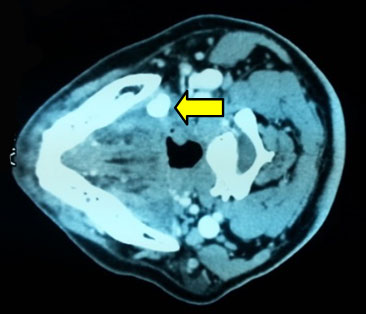
Computer tomography (CT) scan showing salivary calculus (arrow) at left mandible
Management
Diagnosis of salivary calculus is based on clinical examination and imaging. The management of patients with salivary calculus can be divided into immediate and definitive management.
Immediate management
Patients with salivary calculus are sometimes prone to infection at the affected area and require immediate treatment. Usually antibiotics and analgesics will be prescribed. Systemic manifestations of infection such as dehydration secondary to poor oral intake and fever often require hospital admission.
Definitive management
- A small calculus in the duct can be flushed out by increasing the production of saliva. This can be achieved by consuming saliva-stimulating food such as lemon and increasing water intake.
- Calculus that cannot be flushed out spontaneously requires medical treatment. Available treatments are as follow:
- Calculus located near to the duct opening can be gently milked out using finger pressure. This procedure can be done in the clinic setting under local anaesthesia.
- Calculus that is too large to be milked out requires a small incision of mucosa overlying the calculus. Usually the incision site will not be closed with any stitches. This technique can be done both under local or general anaesthesia depending on the size and the location of the calculus.
- Sialoendoscopy can be used for removal of calculus located in the duct. Once the location of the calculus has been identified, a tiny instrument at the tip of the scope such as a micro basket will be used to grasp and remove the calculus. This technique can be performed under local or general anaesthesia depending on the size and location of the calculus
- Repeated infection of the salivary gland secondary to salivary calculus may cause an irreversible damage to the salivary gland and thus require surgical removal. Other instance that necessitates the removal of salivary gland is the presence of calculus within the gland.
- Extracorporeal shock wave lithotripsy (ESWL).
- This technique uses high energy shock wave directed at the calculus to break it into small pieces so that it can be flushed out by saliva.

Picture showing salivary calculus in a surgically removed submandibular gland
Prevention
Although the exact cause of salivary gland calculus is unknown, certain measures such as increase of water intake and eating properly may prevent the incidence of salivary calculus.
References
- Malik, N. A. (2012). Textbook of Oral and Maxillofacial Surgery (3rd ed.). New Delhi: Jaypee
- Myers, E. N., & Ferris, R. L. (Eds.). (2007). Salivary Gland disorders. Pittsburgh, PA: Springer.
| Last Reviewed | : | 13 February 2017 |
| Writer | : | Dr. Logesvari a/p Thangavalu |
| Accreditor | : | Dr. Mukhriz bin Hamdan |







