Introduction
Each person has 2 kidneys situated in the lower back. Each kidney is made up of ~ 1 million tiny filtering units called the “glomeruli”. The glomeruli filter or cleanse our blood continuously to produce urine to remove waste products, salts and excess water from our body. Diseases that affect the glomeruli are called glomerulopathy or glomerulonephritis. When glomeruli become damaged, protein and blood may leak into the urine resulting in proteinuria or hematuria. This may also result in body swelling, high blood pressure and even kidney failure.
Kidney Glomerulus
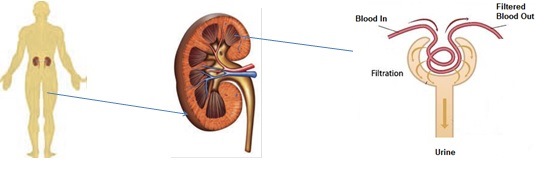
Membranous nephropathy is disease that leads to changes and inflammation of the structures inside the kidney. It is caused by thickening of the glomerular basement membrane which is part of the kidney that helps filter wastes and fluids. The thickened basement membrane does not work normally, hence, leads to loss of large amount of protein in the urine.
Epidemiology
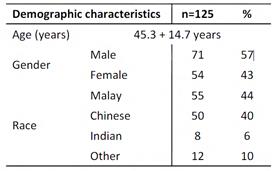
Membranous nephropathy is one type of glomerulopathy that is most commonly seen in adults over the age of 40. From the 2nd Report of the Malaysian Registry of Renal Biopsy, membranous GN accounts for 11% of all primary glomerulonephritis. The mean age at biopsy was 45.3 + 14.7, with a range between 19 and 80.8 years.
Causes
Most cases of membranous nephropathy are “idiopathic” which means we do not know the cause.
Some cases are “secondary” to:
- Drugs eg Penicillamine , timethadione.
- Toxins eg gold and mercury
- Infections eg Hepatitis B, Malaria, syphilis
- Immune diseases eg Systemic Lupus Erythematosus (SLE), Rheumatoid arthritis (RA)
- Cancers eg lung and colon cancer
Symptoms/Presentations
Patients with membranous nephropathy may present with:
- Asymptomatic urinary abnormalities – detection of protein and sometimes blood in the urine without patients experiencing any clinical symptoms
- Oedema or Nephrotic syndrome – body swelling especially around the eyes, feet and hands. This is due to the leakage of large amount of protein in the urine.
- High blood pressure
- Low blood protein level
- High blood cholesterol level
- Impaired kidney function
From the 2nd Report of the Malaysian Registry of Renal Biopsy, the majority (70%) of patients with membranous nephropathy presented with nephrotic syndrome. 22% presented with asymptomatic urinary abnormalities. High blood pressure was found in 21% of cases and 37% presented with impaired kidney function (eGFR< 60mls/min).
Diagnosis
Your doctor will usually order a series of tests and these include:
- Urine tests : to detect protein and blood in the urine, and to quantify the amount of protein leakage in the urine
- Blood tests: to determine the levels of protein, albumin, cholesterol in the blood, to determine the level of kidney functions and to look for possible secondary causes.
- Kidney Ultrasound : to assess the size and structure of the kidneys (especially with impaired kidney function and in preparation for kidney biopsy)
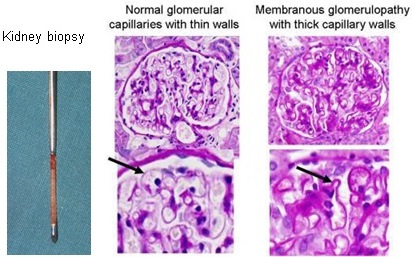
- Kidney biopsy: to get a small piece of kidney tissue for examination under the microscope. Under the microscope, membranous nephropathy is characterised by sub epithelial immune deposits with spikes and thickening of the basement membrane. This test is needed to confirm the diagnosis of membranous nephropathy.
Treatment
Various medications may be given by your doctors and these include:
- Diuretics eg frusemide, spironolactone, hydrochlorthiazide etc: this is to reduce or control the body swelling
- ACE inhibitor or ARB eg perindopril, enalapril, ramipril, losartan, irbesartan, valsartan, telmisartan etc: this blocks the renin angiotensin hormone system and helps to control blood pressure and the amount of protein leakage in the urine
- Other anti-hypertensives eg amlodipine, nifedipine, metoprolol, prazosin etc: this helps to control/lower the blood pressure that may be associated with membranous nephropathy
- Statins eg lovastatin, simvastatin, atorvastatin, pravastatin etc: this helps to lower the blood cholesterol level
- Immunosuppressants eg prednisolone, cyclosporine, azathioprine, cyclophosphamide : these are used in the more severe cases to suppress your immune system and treat the membranous nephropathy
- Anti-coagulants eg warfarin, heparin may be needed: to prevent blood clots from forming
Prognosis /Outcome
The natural history of membranous nephropathy varies greatly. For some patients (~30%), membranous nephropathy may go away on its own with time, without treatment and this is most likely in mild cases.
For another 30%, it may improve slightly or remain stable over many years. In another 30% of cases, it may get worse and result in progressive loss of kidney function with time. These are the patients that need aggressive treatment to stop or slow the disease progression.
The factors associated with higher risk for progression are:
- Male
- Age over 50
- Heavy urine protein loss
- Abnormal kidney function at presentation
- Poorly controlled blood pressure
| Last Reviewed | : | 05 August 2013 |
| Writer | : | Dr. Clare Tan Hui Hong |







